Coronavirus Today: Is COVID-19 the new flu?
Good evening. I’m Karen Kaplan, and it’s Tuesday, Sept. 27. Here’s the latest on what’s happening with the coronavirus in California and beyond.
With the rollout of bivalent boosters, the fight against COVID-19 took a big step toward looking like the fight against seasonal flu.
Every year, the vaccine experts who advise the Centers for Disease Control and Prevention examine the influenza strains in circulation around the world and recommend shots (and sometimes nasal sprays) that target those most likely to sicken Americans that winter. The Food and Drug Administration followed the same principle when it ordered up a new batch of COVID-19 booster shots designed to target BA.5, the dominant version of Omicron, as well as the original coronavirus strain.
Public health officials are urging Americans to get the new boosters now so they’ll be protected in the late fall and winter — the time of year when the pandemic’s two deadliest surges began. That mirrors the annual flu shot campaign, which aims to get people vaccinated in September or October, before the flu season begins in earnest.
No less an authority than Dr. Anthony Fauci has spelled out the similarities between the country’s approach to the two diseases.
“It is becoming increasingly clear that, looking forward with the COVID-19 pandemic, in the absence of a dramatically different variant, we likely are moving towards a path with a vaccination cadence similar to that of the annual influenza vaccine, with annual, updated COVID-19 shots matched to the currently circulating strains,” he said during a White House briefing this month.
Meanwhile, the health officials who have spent years trying to persuade us to wear face masks in indoor public settings are relaxing their recommendations.
California no longer advises everyone to mask up every time they enter a business, government building, cooling shelter or the like unless they’re in a county with a high COVID-19 community level. As of Tuesday, none of them are.
And Los Angeles County, perhaps the country’s most fervent supporter of face coverings, has dropped its mask requirement for public transportation and transit hubs.
If you put it all together, it may be tempting to conclude that COVID-19 has finally become like the flu — an endemic virus that causes inconvenient illnesses and some deaths every year but doesn’t rule our lives.

That would be the wrong conclusion, warns Dr. Peter Chin-Hong, an infectious disease expert at UC San Francisco.
“A vaccination campaign that matches our approach to the flu does not make COVID itself comparable to the flu,” Chin-Hong writes in an Op-Ed for The Times.
Even with all the vaccine doses at our disposal, and even considering all the immunity built up from the roughly 96 million coronavirus infections that have been documented in the U.S., a virus that behaves like BA.5 could wind up killing 100,000 people per year, according to Trevor Bedford, a computational virologist at the Fred Hutchinson Cancer Center. Other experts have put 100,000 annual deaths at the low end of their forecasts.
It would be on the high end for flu deaths — beyond it, in fact. In the decade before COVID-19 came along, the deadliest flu season in the U.S. occurred in 2017-2018, when the country sustained roughly 52,000 deaths, according to the CDC. In other years, the death toll was as low as 12,000.
The gap between COVID-19 and the flu could grow further if a new variant comes along that makes Omicron look tame. With the right combination of mutations, it could erase a good chunk of our hard-won immunity and put us closer to where we were in late 2020 or early 2021.
Plus, the bivalent booster shots have been available for less than a month. It’s way too soon to say whether an annual targeted booster shot will be enough to contain the wily coronavirus.
“If we have learned anything from this pandemic,” Chin-Hong reminds us, “it should be to treat this shape-shifting threat with humility.”
By the numbers
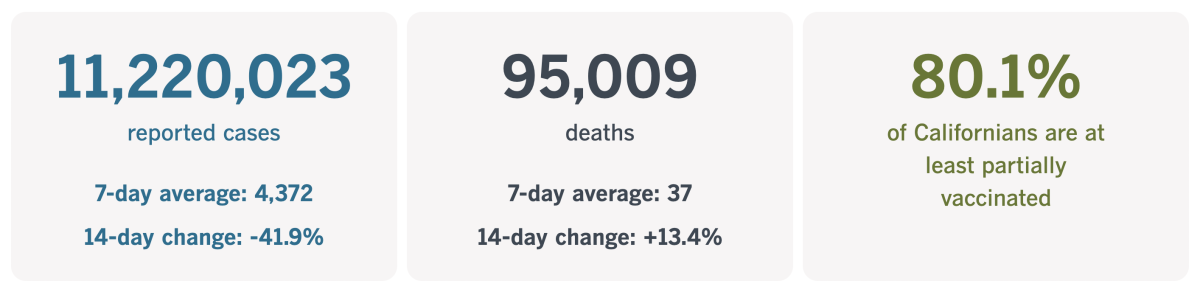
California cases and deaths as of 4:28 p.m. on Tuesday:
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
A pandemic success story
Eight.
That’s the magic number for Kneeland Elementary, one of the smallest public schools in California.
As long as the school has at least eight students enrolled, its future is secure. If enrollment drops below that number, it must get waivers from the state and from Humboldt County to keep its classrooms open.
It may not sound like a high bar, especially since the school teaches kids in transitional kindergarten all the way through eighth grade. That averages out to less than one student per grade level.
But Kneeland is located about a dozen miles east of Eureka, and nearly 300 miles north of San Francisco. As my colleague Hailey Branson-Potts writes, it’s not so much a town as “a rural fire station and a smattering of homes in the forest.” With such a tiny population to draw upon, mustering up eight students isn’t necessarily a given.
During the 2018-2019 school year — the last normal year before the pandemic — Kneeland Elementary had an average daily attendance of 13. That triggered a recruiting campaign. The two teachers covered the school bus in colored lights for a Christmas parade in Eureka. Students in grades four through eight wrote a play called “Everyday Heroes” and performed it in Ferndale, about an hour’s drive away.
They didn’t know it at the time, but they were about to get a huge recruitment boost courtesy of the pandemic.
Kneeland Elementary is so small that it was able to reopen while other schools struggled with distance learning. Its 2.5-acre mountaintop campus offered plenty of space for outdoor classes, including a biology unit on bugs. When it was necessary to be indoors, the low headcount meant social distancing wasn’t much of a challenge.
That doesn’t mean the school was blasé about COVID-19 precautions. On the contrary, the tiny school had a huge incentive to take them seriously.
“If teachers get sick, we don’t have any substitutes,” said Cherie Circe, the district secretary.

Parents in the surrounding area took notice that Kneeland was teaching classes in person. One of them was Nicole Quinlan, whose son Asha lost his spirit after the 400 kids at his elementary school near Arcata were forced to go online.
Asha used to be outgoing, with a quick wit and contagious giggle. But distance learning was onerous for the rural Quinlan household, where internet service was dicey and Asha was overtaken by loneliness.
“We gave it a fair shot,” Nicole Quinlan said, recalling her son’s tears. “I’m not being dramatic — it was traumatizing.”
She secured an interdistrict transfer for Asha even though it meant 90 minutes of travel time each school day. His commute involves a 15-minute drive to a bus stop, followed by a half-hour bus ride on a mountain road. Yet when offered the choice to go back to his old school this year, the sixth-grader’s answer was, “Oh, heck no.”
He’s not the only convert. Third-grader Bailey Gingerich transferred to Kneeland with her older sister during the pandemic, and now she can’t imagine attending school anywhere else.
“You’ll never run out of oxygen because you can just go near a tree,” she said. “We’re in nature, and everybody’s nice.”
The school’s enrollment has nearly tripled, with 33 students. Kneeland hired a third teacher and built a new classroom.
“These fabulous families recognized how unbelievably awesome we are, and stayed, which thrilled us to pieces,” said Greta Turney, the school district’s not-exactly-impartial superintendent who also teaches sixth through eighth grade.
Kneeland’s experience stands in marked contrast to the state as a whole. Public school enrollment has plummeted across California in the last five years, with the biggest drop coming after the onset of the pandemic.
Students and teachers aren’t the only ones pleased to see Kneeland Elementary buck the trend.
Mark Moore, a 67-year-old rancher and logger who attended the school as a boy, dropped by while Branson-Potts was there. Moore sent his own children to Kneeland and now has two grandchildren enrolled, with a third slated to start next year. He said it was life-affirming to visit the school and hear the students’ “happy banter.”
California’s vaccination progress
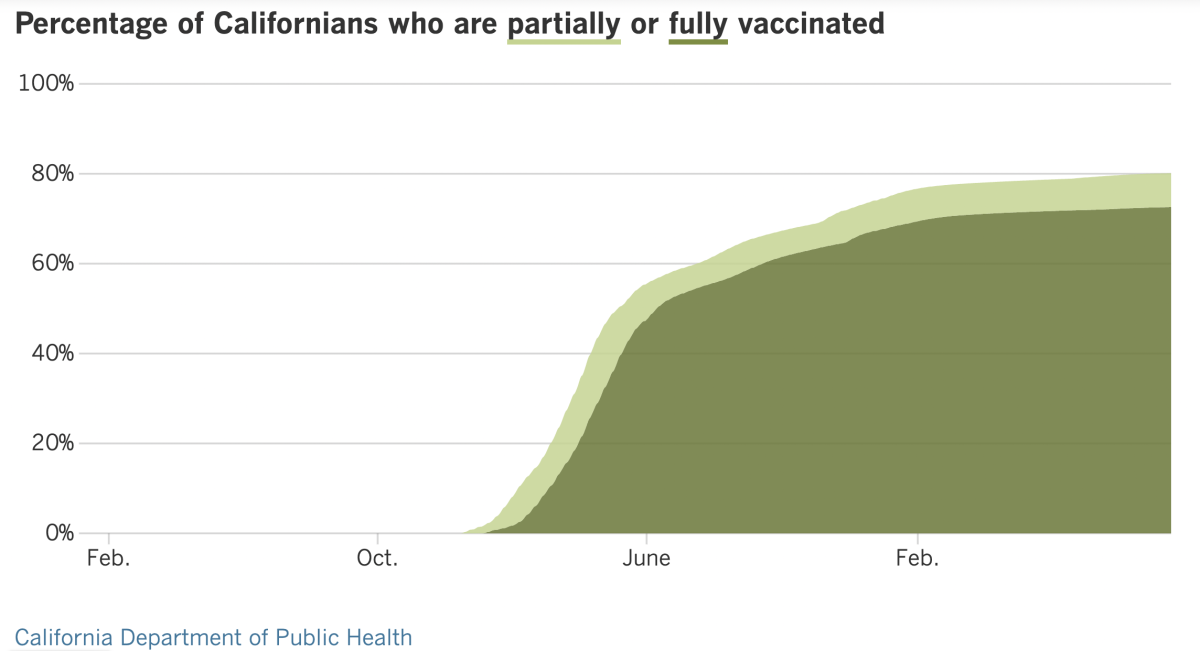
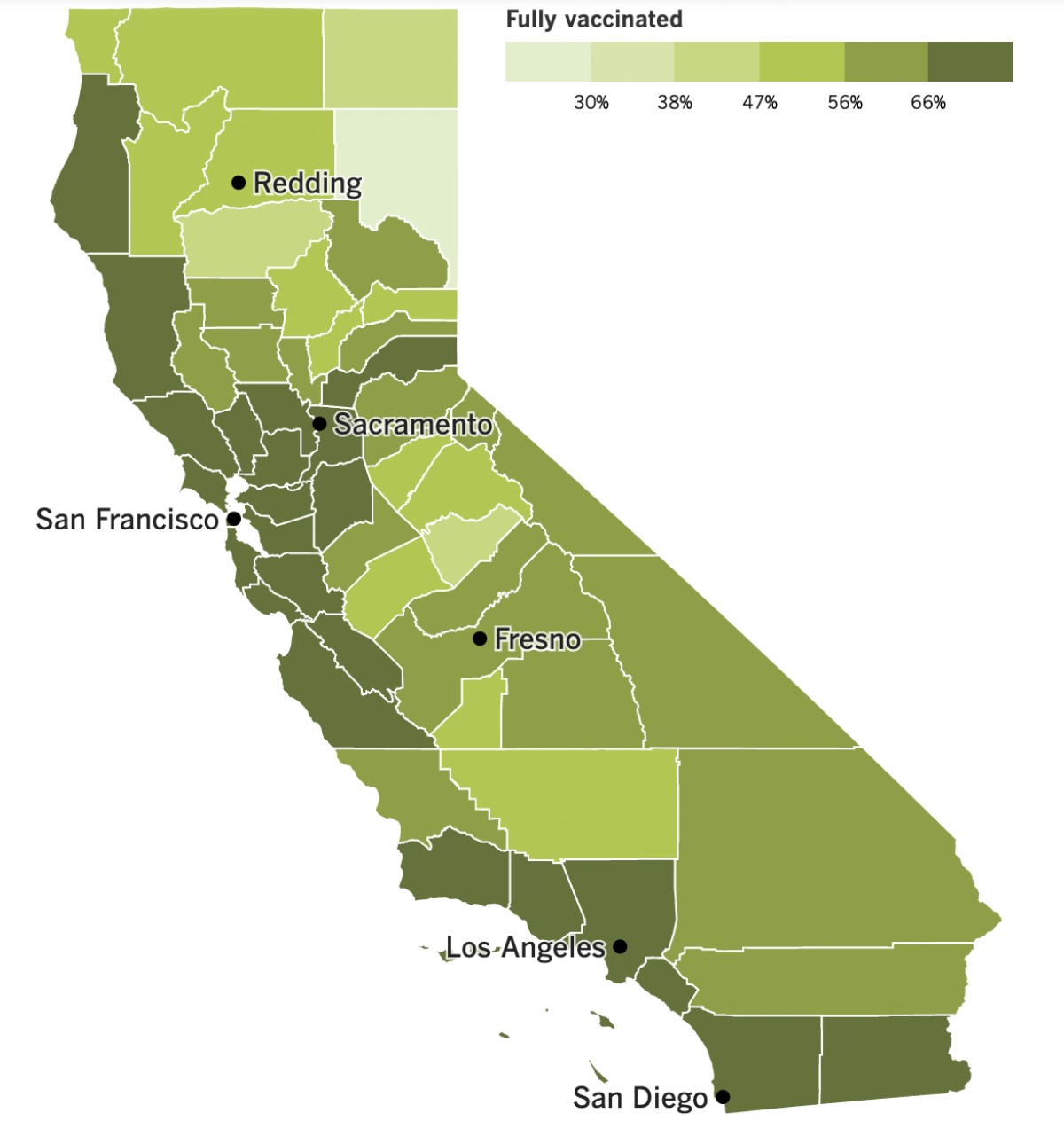
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
As mentioned earlier, California health officials have eased their guidance on face masks in light of the state’s improving coronavirus conditions. It’s the first time the recommendations have been relaxed since mid-February, when the whole country was recovering from the record-breaking Omicron surge.
As of Friday, the California Department of Public Health recommends universal indoor masking only in counties with a high COVID-19 community level. Eight of the state’s 58 counties — Kern, Merced, Stanislaus, Mariposa, Tuolumne, Glenn, Butte and Tehama — are currently in the “medium” category and the rest are classified as “low.”
That means workplaces, retailers, government offices and entertainment centers throughout the state can make their own decisions about whether to require masks. And in the counties with a low COVID-19 community level, higher-risk facilities like homeless shelters and jails can make their own rules as well. (When the COVID-19 community level is “medium,” masks are required in these higher-risk settings.)
If you’re in a venue that leaves the masking decision up to you, the state’s advice is to “consider wearing a mask” if you’re in a county with a medium COVID-19 community level, and to go with your “personal preference” if you’re in a county with a low community level. If you’re considered vulnerable — that is, you have a chronic health condition that increases your risk of becoming severely ill with COVID-19 — the state recommends masking up in crowded indoor spaces if the community level is “medium” and advises you to consider doing the same if the community level is “low.”
Masks are still required statewide in all healthcare facilities and long-term care centers, regardless of the COVID-19 community level.
Counties are allowed to adopt stricter rules. But in Los Angeles County, the rules are going the other way. As of Friday, the local health order no longer mandates the use of masks on buses, trains, in Ubers and Lyfts, or in airports or other transit hubs.
L.A. County Public Health Director Barbara Ferrer said face coverings are still strongly recommended for travelers, even if they’re not required. “From our perspective,” she said, “it’s a great idea to keep your mask on.”
But the mandate was put in place to protect transit workers, and with coronavirus transmission levels so much lower than in the past, health officials said the time had come to relax the health order.
Now the number of California counties with transit-specific mask rules is zero. However, the operators of the Bay Area Rapid Transit system still have a mask mandate in place through the end of the month. Masks are also required on AC Transit, which provides bus service in the East Bay.
The relaxed rules reflect just how much cases have dropped since the height of the BA.5-fueled surge. According to The Times Tracker, the daily case count (measured as a seven-day average) has dropped more than 40% over the last two weeks alone, while the daily death toll has been holding steady at a level not seen since before the Delta variant hit.
Sadly, there’s no guarantee these conditions will last.
“Enjoy the good ‘COVID weather’” while it’s here, Chin-Hong said, because there are already signs that worse days may be on the horizon.
One of those signs comes from Europe, where case rates are starting to tick up in some countries. In England, for instance, infections have increased 13% week-to-week and hospitalizations rose 17%. Numbers are also starting to climb in Belgium and Denmark, Chin-Hong said. If a surge materializes across the pond, there’s a good chance one will follow here.
Another vexing sign comes from L.A. County’s wastewater monitoring system, which indicates coronavirus levels are holding steady instead of falling. “The fact that we’re no longer seeing decreases in wastewater data is a reminder that transmission remains substantial across the county,” Ferrer said.
And then there’s the fact that cooler weather — it’s bound to arrive eventually — will prompt people to spend more time together indoors. That will make it easier for the coronavirus to spread, especially if there are new variants.
BA.5 is still the dominant strain in the country by far, but its market share has been slipping for weeks. It now accounts for an estimated 83.1% of coronavirus specimens circulating in the U.S., according to the CDC.
The Omicron subvariant working hardest to take its place is BA.4.6, which now makes up about 11.9% of viral specimens, up from about 7.8% in late August, the CDC says. In third place is another subvariant known as BF.7, which accounts for 2.3% of coronavirus strains in the U.S.
These are all reasons why infectious disease experts took President Biden to task for prematurely claiming “the pandemic is over” on “60 Minutes” this month.
“We’re already hearing pushback: ‘If it’s over, why do I need a booster?’” said Dr. Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota.
A version of that is happening in Congress, where Republicans asked why they should approve Biden’s request for $22.5 billion in additional funding for coronavirus tests, vaccines and treatments if the pandemic is over. (Full disclosure: They’d been opposed to the funding request long before the TV show aired.)
“We have to continue to make the case that COVID is still a threat,” said Dr. Robert Wachter of UC San Francisco. “We still need to encourage people to get a booster. And we need Congress and other policymakers to see ongoing funding as important, including funding for finding a new vaccine and research on long COVID.”
Speaking of vaccines, Pfizer has asked the Food and Drug Administration to authorize its bivalent booster for children ages 5 to 11. The shots feature a kid-sized dose of the vaccine that is already authorized for Americans 12 and up. Dr. Peter Marks, the FDA’s vaccine chief, has said he expects to see action on updated boosters for school-age children “soon.”
The company and its partner, BioNTech, also said they’ve begun a new trial of their bivalent booster for infants, toddlers and preschoolers. The study’s aim is to figure out the optimal dose for children ages 6 months through 4 years.
There’s good news for Americans looking to travel. Canada said Monday that its COVID-19 vaccination requirement for people entering the country will be dropped at month’s end. And if you’re flying into the land of poutine and maple syrup, you’ll no longer have to wear a mask on the plane.
Heading to Asia? Hong Kong has dropped its requirement that visitors quarantine in designated hotels upon arrival. Instead, they can monitor themselves at home for three days, and if they test negative at that point they’ll be free to roam. They’ll still have to follow a regimen of mandatory PCR tests and rapid antigen tests during their first week.
Taiwan may relax its quarantine rules as well. Officials said they may replace quarantine with seven days of self-health monitoring in mid-October. A decision is expected this week.
Your questions answered
Today’s question comes from readers who want to know: Does it matter which bivalent booster shot I get?
In a word: No.
This is not like your primary vaccination series, where if you got the Pfizer-BioNTech vaccine the first time, you had to get a Pfizer-BioNTech shot the second time. (Ditto for the Moderna vaccine.) Once you’ve got those initial doses under your belt, you can either stick with the same brand or switch to the other.
Either way, you won’t be getting the same shot you had last time. That’s because your last booster targeted only the original coronavirus strain, while the new bivalent boosters for adolescents and adults add protection against the BA.4 and BA.5 versions of Omicron.
Both Pfizer and Moderna have versions of the bivalent booster. Moderna’s is authorized for all adults 18 and up. Pfizer’s is authorized for adults and adolescents 12 and up. So if you’re in the 12-17 age group, you have to get the Pfizer vaccine because it’s your only option. (Those under 12 will have to wait a little longer for a bivalent booster to become available.)
Adults can go either way. Some people might feel more comfortable sticking to the brand they’ve had before, while others may feel that mixing things up is a good way to hedge their bets. Scientists have not found any downside to a mix-and-match strategy, and in clinical trials, people who switched brands for their booster shot often produced more antibodies than people who didn’t.
The pros and cons of mixing and matching haven’t been studied with the bivalent booster, but experts say the calculus should be the same. The most important part of the equation is to get a bivalent booster when you are eligible, regardless of the brand.
“The best booster for you is the one that you can get,” Dr. Robert Kim-Farley, an epidemiologist and infectious disease expert at the UCLA Fielding School of Public Health, told my colleagues Luke Money and Rong-Gong Lin II. “If there’s shortages of one, you should not have hesitancy to take the other.”
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The woman in the photo above is Shamita Jayakumar. She’s a 32-year-old tech worker who finds refuge from pandemic stress by shopping at Target.
Her biweekly trips to the cheap-chic retailer have become a form of self-care. And she’s got lots of company among Gen Z, millennial and Gen X women who can afford to splurge on a $20 sweater or a $25 kitchen gadget while picking up necessities like toothpaste and milk.
Google searches for “self-care” shot up during the initial pandemic lockdown period, then again during the first Omicron surge.
“If it brings you joy to do it, that’s your self-care,” Desiree Rew, a clinical social worker in Long Beach, told my colleague Marisa Gerber.
An item emblazoned with the message “GOOD VIBES” may sound cheesy, but it can also be inspirational, she said: “Yes, they want good vibes. We’ve been surrounded by bad vibes.”
Resources
Need a vaccine? Keep in mind that supplies are limited, and getting one can be a challenge. Sign up for email updates, check your eligibility and, if you’re eligible, make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




