Multipronged vaccine protects against COVID virus family members — even some still in hiding
Long before COVID-19 transformed daily life, scientists were aware of the possibility that a coronavirus could make the leap from an animal species to the human population.
How different the last few years might have been had a vaccine capable of blocking the SARS-CoV-2 virus been administered to workers at the Huanan Market in Wuhan, China — where, scientists suspect, a raccoon dog infected a vendor and set off a pandemic that has killed more than 6.3 million people around the globe.
A new type of vaccine developed at Caltech aims to ward off novel coronaviruses even before health officials are aware that they exist. When tested in mice and monkeys, it trained the animals’ immune systems to recognize eight viruses at once — and induced immunity to viruses they had never encountered.
The findings, published Tuesday in the journal Science, could lead to a powerful tool against a virus that mutates too quickly to be contained with current vaccines. An international vaccine foundation has pledged $30 million to begin clinical trials of the experimental vaccine in humans.
“We’ve had three pandemics or epidemics in the past 20 years: first SARS, then MERS, then SARS-CoV-2,” said Caltech biochemist Pamela Bjorkman, who led the new work. More outbreaks sparked by “spillover events” are inevitable, she said, and “we want to protect now against the future spillover.”
Dr. Anthony Fauci, President Biden’s chief advisor on the COVID-19 pandemic, praised the research as “a major conceptual step toward a pan-coronavirus vaccine.”
“It’s a very, very important proof of concept,” he said, noting that it remains to be seen whether it works as well in humans as it has in lab animals. “That’s why you do the experiment.”
A young Briton agreed to be infected with the coronavirus for a scientific study of the most consequential virus on the planet.
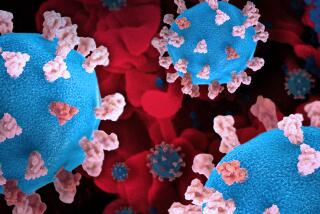
The new vaccine doesn’t block all coronaviruses, an ambitious goal not yet within science’s grasp. Instead, it focuses on the group known as betacoronaviruses, which includes those that cause COVID-19, severe acute respiratory syndrome and Middle East respiratory syndrome, among other diseases.
Rather than using a piece of inactivated virus or a lab-created molecule designed to mimic one found in nature, the Caltech researchers created a microscopic speck of matter that they could adorn as they pleased. Their nanoparticle is composed of proteins with sticky bits on their surfaces, to which researchers can attach even tinier bits of viruses.
The team tested three versions of the nanoparticle. One was covered with pieces of SARS-CoV-2. A “mosaic” version had SARS-CoV-2 plus samples of seven other coronaviruses, including one that causes MERS and other strains found in bats and pangolins. The last one was bare, to serve as a control.
When looking for pieces of viruses to clip and attach, the team zeroed in on a section of the spike protein called the receptor binding domain, or RBD. This is the part that’s typically targeted by the immune system’s neutralizing antibodies, whether they’ve been generated in response to a vaccine or a previous infection.
Given that the RBDs of betacoronaviruses share many characteristics, the researchers hoped that the mosaic version would prompt the immune system to focus on parts common to all eight viruses. They further theorized that if these parts were shared across most or all betacoronaviruses, the vaccine would trigger an immune response when presented with any member of the viral group — even those that weren’t among the samples.
They were right.
Newfangled COVID-19 vaccines have left many people yearning for an old-school alternative. The one from Novavax could fit that bill.
As they designed their mosaic nanoparticle, they deliberately left out SARS-CoV, the virus responsible for severe acute respiratory syndrome. If the vaccine worked as intended, animals vaccinated with the mosaic nanoparticle, then exposed to SARS-CoV, would mount an immune response.
They did. In fact, the vaccinated mice and monkeys had little to no detectable virus in their systems despite attempts to infect them with either SARS-CoV or SARS-CoV-2.
“We’re very excited about that,” Bjorkman said.
That wasn’t the case with the animals injected with the bare nanoparticle — they weren’t able to fight off any viruses and died. The animals that received the vaccine with pieces of SARS-CoV-2 only were protected against that virus but had no protection against any other coronavirus, and most of them died as well.
If the mosaic vaccine works as well in humans as it did in animals, it could offer protection against the betacoronaviruses we know about, as well as related ones that have yet to make the leap to humans.
That prospect is promising but far from certain.
With immunity waning and the Omicron variant looming, many scientists are saying the definition of ‘fully vaccinated’ should include a booster shot.
The next step is a Phase 1 clinical trial in humans, the first hurdle to cross when bringing a new drug or vaccine to market in the U.S. That will take place at Oxford University, home to Bjorkman’s collaborators on the project, and will likely take at least a year.
The Coalition for Epidemic Preparedness Innovations said Tuesday that it will foot the bill for the initial trial, with the goal of establishing evidence that the vaccine is safe in humans.
“It’s certainly encouraging,” said Dr. Paul Offit, a virologist and immunologist at the University of Pennsylvania. “But these are animal model studies, and as is well known among scientists, mice lie and monkeys exaggerate.”
“It’s hard to make universal vaccines work,” Offit added. “It’s not for want of money. It’s not for want of desire or effort. It’s just a very hard thing to do.”
Scientists and their funders should throw the same effort into fighting the virus’ future as they did in its early days.
This isn’t the only team in the U.S. exploring nanoparticle vaccines for coronaviruses. Researchers at Duke University and the Walter Reed Army Institute of Research are investigating them as well.
“These general approaches all use the receptor binding domain to elicit strong antibody responses that can neutralize the virus, so they all have some promise,” said Dr. Stanley Perlman, a virologist and immunologist at the University of Iowa who specializes in betacoronaviruses.
“This is a good approach based on what we know,” he said, “and one has to hope that it’ll be useful for viruses that we haven’t identified yet.”