Op-Ed: What will it take to make a universal COVID vaccine?

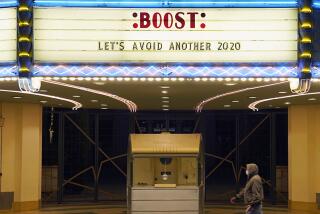
As California emerges from Omicron, other places are again in lockdown or facing record caseloads after trying and failing to avoid the variant. Many of us who did everything right, getting every shot and booster and avoiding crowds, nonetheless got infected.
COVID’s persistence could push us toward a concession to just live with the virus. But that seems defeatist, and is perilous. Highly infectious variants erupted from parts of the world that still have low vaccination rates and high population density. New research finds accelerated cognitive decline and cardiovascular problems after even mild COVID infections. Over a dozen animal species are now known to be infected with SARS-CoV-2, setting the stage for new mutations. We need a new approach, now, to defeat future waves of this virus and other viruses that might emerge.
That points to a lifelong, durable, broadly protective vaccine. What will it take to develop one? It will be a tough road, but it’s possible. Success will require two principles that the world has not yet sufficiently grasped in fighting this virus: a focus on the long term over the short term, and a sustainable structure and support for collaboration.
Facing its worst outbreaks since 2020, China could use help from the U.S.
One challenge is that there are so many viral sequences the vaccine has to protect against, arising not only from emerging SARS-CoV-2 variants, but also from the multitude of other coronaviruses that may yet spill into humans. The first-generation mRNA vaccines, which teach the body to recognize the spike protein part of the virus and mount an immune response, encode a viral strain that no longer circulates. Since this protein is so prone to mutation, making it harder for the body to recognize in future variants, a more universal vaccine must target parts of the virus that are shared among several viruses in the family — often essential components that are less likely to mutate.
Unfortunately, these parts are often less noticeable by the immune system. Science has since found better ways to prompt a more effective immune response to the spike protein, and better ways to engineer and display that protein itself, but finding the right combination of the different strategies will take coordination.
And we’re not sure if the mRNA format, which emerged as a vaccine strategy after decades of development, is best against the next new pathogen, compared with other vaccine approaches such as using nanoparticles that allow more options for vaccine formulations, weakened or killed viruses, or viral vectors that contain a greater variety of molecules and may trigger protective viral-sensing mechanisms.
To handle these complexities, we’ll need all kinds of experts — including in developing novel vaccine formats to elicit an effective, long-lasting immune response and in understanding the vaccine components that cause immune cells to spring into action. We need experts that understand how antibodies don’t just inactivate the virus, but also recruit an army of complementary immune cells to clear the pathogen from the body. We also need experts in preclinical models to help us understand which vaccine candidates to advance to human trials, and how to gauge their success. And we need experts in large-scale vaccine production, cost and distribution logistics.
A study of healthcare workers finds that a second booster dose of Pfizer’s COVID-19 vaccine did little to prevent Omicron infections.
Each of these hurdles will be addressed by distinct groups of scientists, each working in a different discipline and at a separate site. The right vaccines probably won’t be made by one group or company alone but will result from a concerted effort of many approaches that overcome different variables. So globally, researchers will have to collaborate on the scale and style of the Manhattan Project to build a lasting solution. Since researchers have already arrived at better solutions than the approaches in early 2020, they have plenty to start with. Many labs are already pursuing different routes to a universal vaccine.
The scientific enterprise, however, is built on competition, not mass collaboration without regard to your individual career. Competition has benefits: It encourages innovation, driving us to get results faster and to deliver a better result or product than that of our competitors. The downside is the lack of sharing — of results, samples and crucial insights. Competition for limited funding and the need to publish results first can lead to siloing and a focus on rapid results instead of thorough ones.
It is easy to call for sharing and coordination, but that call will go ignored without structures to support and encourage researchers. Both of us know this firsthand: We’ve been involved in building large, multidisciplinary collaborative efforts among competitors to untangle research problems no single lab could attempt alone. This required creating and revising systems to develop and evaluate competing ideas or treatments simultaneously, backed by data-driven machine-learning approaches that evaluated results on a level playing field. These approaches made it possible to understand why some antibodies were protective and others weren’t, and what laboratory experiments best identified those treatments that would be successful in people.
Our collaborative approaches worked because they set up individual labs to succeed, while also contributing to the greater good. Participating lab researchers needed to have publishable papers come out of the projects, so that contributing their time and effort would advance their career instead of costing it. They also needed protection of their intellectual property, so they were able to participate and share, alongside funding to support work on a greater scale or depth than their current funding sources would permit.
Drugmaker Moderna asked the Food and Drug Administration to authorize a fourth shot of its COVID-19 vaccine as a booster dose for all adults.
Companies that gave access to their researchers and supplies, meanwhile, needed tangible benefit: They would receive valuable data that they could use for new drug filings, and the consortium’s work would open new doors for their products. The federal and philanthropic funders of these projects also received strong bang for their buck: a body of knowledge that bridged barriers and advanced the field as a whole.
Motivating philanthropic and federal funders will be essential to develop longer-lasting, broadly protective vaccines. Since vaccines typically don’t make much money — a good lifelong vaccine might be administered once, and for much of the world it needs to be donated — federal governments and large philanthropic organizations have to front most of the investment.
They may not feel motivated to continue right now: While earlier in the pandemic the U.S. government and other funders were driven by a sense of immediate crisis, now the focus is on widespread reopening. They may be less willing to prevent what now feels like a potential crisis. Funding and interest in developing vaccines for 2003’s SARS-CoV-1 dissipated after that virus went away; in 2020, we could have used that knowledge and the drugs that would have resulted.
Beyond the continued health risks of COVID, the economic argument for more vaccine investment is hard to dispute. The cost of the SARS-CoV-2 pandemic is an estimated $16 trillion, or nearly 90% of the U.S. GDP. The cost of developing a typical vaccine, more like $1 billion, is 0.006% of that. Even a $10-billion vaccine is minuscule compared with the pandemic’s toll. We can’t afford not to do better.
Erica Ollmann Saphire is president, CEO and professor at La Jolla Institute for Immunology. Edward Scolnick is core member emeritus at the Broad Institute of MIT and Harvard and former head of R&D at Merck Research Laboratories.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.