Scientists have a promising new approach for treating drug-resistant tuberculosis
In research that promises a new approach to treating an age-old human scourge, scientists have found a way to weaken the bacterium that causes tuberculosis and boost its vulnerability to drugs that are rapidly losing their power to cure.
A study published Wednesday in the journal Science and Translational Medicine outlines a new assault against TB by a team led by researchers from Weill Cornell Medical College in New York.
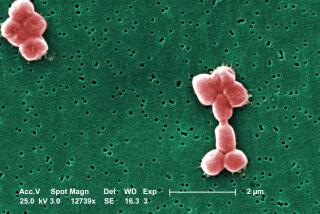
Its aim: to disrupt the production of the TB bacterium’s waxy outer shell and make the pathogen vulnerable to a host of hostile forces, including antibiotic medicines whose effectiveness has begun to wane after years of misuse.
In petri dishes, an agent that disrupted the formation of the TB bacterium’s fatty protective coating not only delivered a lethal blow, it suppressed the bacterium’s penchant for finding a way to bounce back.
And in mice infected with tuberculosis, exposing TB’s innards had a more subtle effect: It boosted the killing power of rifampicin, the antibiotic that is a first-line of defense against TB.
“The intriguing insight here is a strategy for what to target in the bacteria,” said Dirk Schnappinger, a professor of microbiology and immunology at Weill Cornell Medical College and senior author of the new study. “It doesn’t have to be this particular model and it doesn’t have to be this particular enzyme.” A prospective drug might use another of those enzymes to disable TB’s ability to cloak itself in a waxy outer membrane.
That’s important, Schnappinger said, because in the search for a new TB drug, researchers will also have to establish that an experimental candidate will work well with others already in use.
The research promises to open a new front in the battle against a wily and resilient foe that has tormented humans for all of recorded history.
Mycobacterium tuberculosis can hide in the body undetected by the immune system for years, then awaken to shred the lungs of its victim, and spread easily to other victims.
Tuberculosis still infects more than 10 million people worldwide. It kills someone every 15 seconds, claiming 1.3 million lives in 2016.

In the last decade, a determined effort to bring TB under control has come under increasing threat from the rise of antibiotic-resistant strains of the bacterium.
That rise has been driven in part by the difficulty of treating TB: It can take six to eight months of intensive drug therapy to banish the bacterium that causes the disease. And when a patient fails to complete the treatment — a common occurrence — the result can be the emergence of a new and more powerful strain resistant to existing medicines.
The World Health Organization has estimated that in 2016, some 600,000 cases of tuberculosis were resistant to at least two of the front-line drugs used to treat tuberculosis, rifampicin and isoniazid. And public health experts are haunted by the growing prospect of extensively drug-resistant TB, which can’t be vanquished even with four or more medications.
So a therapy that could shorten treatment time, increase the effectiveness of front-line drugs or simply kill TB on its own would be a major step forward.
Even more important, experts say, would be the discovery of an approach that works by means entirely different from drugs already available to treat tuberculosis.
On all those fronts, the new study offers real hope, said Dr. Peter Small, founding director of Stony Brook University’s Global Health Institute in New York.
“This is big news, and I am hopeful that they’re onto something,” said Small, who wasn’t involved in the new research. But, he added, “it’s likely to be years before we know for sure.”
The last decade has seen the introduction of a sensitive new diagnostic test for TB and the discovery of four novel compounds capable of attacking tuberculosis bacteria in new and different ways.
With these have come the high-level attention that tuberculosis has always lacked, Small said. In 2014, the World Health Assembly laid plans for the eradication of TB, and in a first, heads of state will gather at the United Nations in September to endorse that goal.
But in the fight against tuberculosis, as with any infectious disease, “if you are not making progress, you are losing ground,” he said. “Just to stay ahead of antibiotic resistance, we need to constantly introduce new drugs.”
By identifying a fresh target for therapy — the TB bacterium’s waxy outer jacket — the new research lays the groundwork for adding to the armamentarium against TB, said Dr. Marcus Horwitz, a UCLA infectious disease expert and longtime TB researcher. Against a bacterium as complex as tuberculosis, that is no small feat, he noted.
The TB bacterium has about 4,000 proteins, and all of them are potential targets for new drugs, said Horwitz, who was not involved in the new study. “This one they’ve shown is important because when they knock it out, and the organism doesn’t grow well.… They’ve found one that actually does make a difference.”
While the new approach may someday make rifampicin work better, the study authors will need to explore better ways to create a drug that will survive in the body and stay active long enough to make a significant impact. Achieving an acceptable level of “bioavailability” may be one of the key challenges to translating the new discovery into drugs that can make a difference against TB, Horwitz said.
MORE IN SCIENCE
A pileup of 14 distant galaxies is set to become the most massive structure in the universe
This engineered painkiller works like an opioid but isn’t addictive in animal tests
In human cells, scientists find DNA that looks like a twisted knot instead of a double helix