Quick start to HIV drug treatment can cut risk of illness, death in half
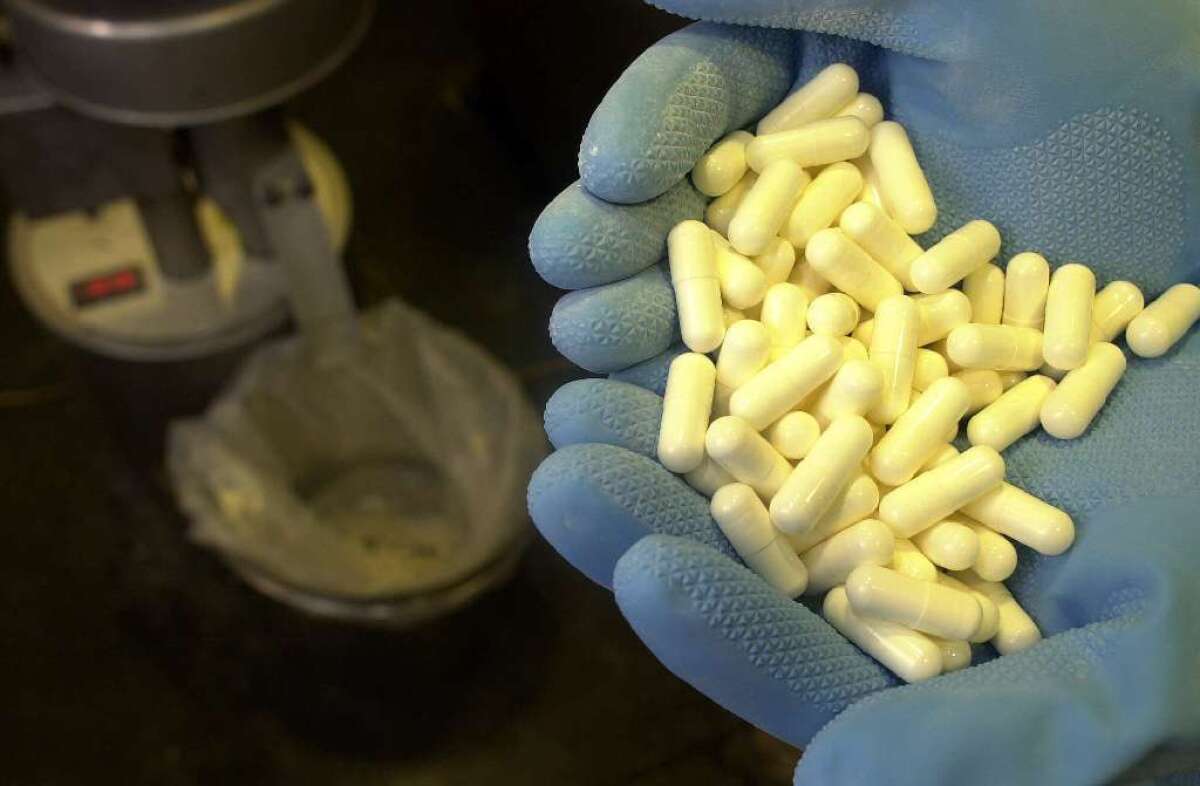
A large clinical trial confirms that HIV-positive patients are less likely to become seriously ill or die if they begin treatment with antiretroviral drugs right away. Above, capsules of the antiretroviral drug Indinavir.
An international clinical trial involving nearly 5,000 people with HIV confirms that treatment with antiretroviral drugs should begin sooner rather than later, the National Institutes of Health announced this week. In fact, the benefits of early therapy were so clear that the study was stopped early so that everyone in the trial could receive the drugs.
Participants in the Strategic Timing of AntiRetroviral Treatment, or START, study who initiated treatment when their immune system was still strong were 53% less likely to die or develop a serious illness compared with those who delayed treatment until their immune systems had been weakened by the human immunodeficiency virus.
People diagnosed with HIV in the United States already start treatment at an early stage, when their count of CD4+ T-cells is still above 500 per cubic millimeter of blood. (The CD4+ count for a healthy adult ranges from 500 to 1,200 cells/mm3.) But doctors had no firm evidence that this approach was better than delaying treatment until a patient’s CD4+ count had dropped below 350 cells/mm3.
“We now have clear-cut proof that it is of significantly greater health benefit to an HIV-infected person to start antiretroviral therapy sooner rather than later,” Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Disease, said in a statement.
When the START trial began in 2011, Fauci and other medical experts were unsure whether the benefits of early treatment would outweigh the risks. Some epidemiological studies suggested that patients had better outcomes when they started therapy sooner. But no one knew whether patients would suffer side effects from being on antiretroviral drugs for a lifetime, or whether early treatment would help HIV develop resistance to the medications.
So the International Network for Strategic Initiatives in Global HIV Trials, a group funded by the NIAID, launched the randomized clinical trial to get a definitive answer.
For the trial, researchers recruited 4,685 HIV-positive adults from 215 sites in 35 countries. All of these men and women had CD4+ counts above 500 cells/mm3 when they joined the study, and none had taken antiretroviral drugs.
About half of these volunteers were randomly assigned to begin treatment right away, and the rest waited until their CD4+ count dropped below 350. Researchers checked in with study participants once every four months.
Between March 2011 and March 2015, 86 members of the deferred treatment group developed serious AIDS-related complications, other serious medical problems (such as major cardiovascular disease and cancer), or died. That compared with 41 such cases among study volunteers who began treatment right away.
They study’s independent data and safety monitoring board calculated that early treatment reduced the risk of serious health problems or death by 53%. Members of the early treatment group were less likely to develop both AIDS-related and non-AIDS-related conditions, though the reduction in risk was greater for complications related to AIDS, the board found.
These benefits were seen in study volunteers from all parts of the world, and the results held up regardless of whether people lived in low-income, middle-income or high-income countries.
Early therapy also helped reduce the spread of HIV from infected individuals to their uninfected partners, Fauci said.
The National Institutes of Health recommends that patients begin taking antiretroviral drugs as soon as they are diagnosed with HIV, regardless of their CD4+ cell count or whether they have any symptoms of infection.
The World Health Organization advises patients to start treatment when their count drops to 500 cells/mm3 or lower. However, next week a WHO panel will meet in Geneva to reassess its guidelines on when to start antiretroviral therapy.
The study’s findings “are likely to influence how care is delivered to millions of HIV-positive individuals around the world,” James Neaton, the study’s principal investigator at the University of Minnesota, said in a statement.
The START study was funded by various parts of the National Institutes of Health, the National Agency for Research on AIDS and Viral Hepatitis in France, Germany’s Federal Ministry of Education and Research, the European AIDS Treatment Network and government organizations in Australia, Denmark and Britain. Medications used in the trial were donated by AbbVie Inc., Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline/ViiV Healthcare, Janssen Scientific Affairs, and Merck Sharp & Dohme.
For more medical news, follow me on Twitter @LATkarenkaplan and “like” Los Angeles Times Science & Health on Facebook.







