Gene therapy offers long-term treatment for mice with diabetes
The newly resurgent field of gene therapy, which recently produced treatments for blood cancers and blindness, has taken a step toward fighting a scourge that is on the rise worldwide: diabetes.
In research reported Thursday in the journal Cell Stem Cell, scientists showed that a single infusion of a virus containing two handpicked genes restored normal blood sugar levels in mice with Type 1 diabetes.
Although the effects of the therapy faded after four months, prompting the mice to return to their diabetic state, the equivalent improvement in humans could last for several years, the researchers said.
Type 1 diabetes occurs when the immune system attacks the beta cells in the pancreas that make insulin, a hormone needed to metabolize the sugar in foods. In Type 2 diabetes, the pancreas can still make some insulin but the body isn’t able to use it properly.
The experimental therapy aimed to tweak one type of pancreatic cell to make it step into the role of similar cells that are destroyed in diabetic patients.
The plan was to introduce two genetic changes into a group of cells known as alpha cells. Once their DNA was modified, the alpha cells would take over the job of making insulin.
When scientists used a bioengineered virus to introduce the two changes into human cells in the lab, the pancreatic alpha cells took on the insulin-producing function normally assigned to beta cells.
When tested in mice, the alpha cells modified by the experimental therapy did the same thing, allowing the animals to keep their blood sugar in check.
Dr. George K. Gittes, a University of Pittsburgh pediatric surgeon and the senior author of the new study, said he and his colleagues have already seen some success in testing the experimental therapy in non-human primates. Next, he said, his team will seek permission from the Food & Drug Administration to launch clinical trials using the viral gene therapy in patients with Type 1 and Type 2 diabetes.
That effort comes at a pivotal time both for gene therapy and for diabetes, a metabolic disorder that has nearly doubled in prevalence across the globe since 1980.
In announcing the approval in late December of a gene therapy to treat an inherited form of blindness, FDA Commissioner Scott Gottlieb touted the approach as one that “will become a mainstay in treating, and maybe curing, many of our most devastating and intractable illnesses.”
Until recently, using a virus to ferry genetic fixes to their targets has caused illness and death in patients. But advances in genetic engineering have made it possible to disarm viruses of their ability to sicken people without compromising their knack for sneaking into cells and altering their DNA.
With hundreds of experimental gene therapies now under development, Gottlieb said he has committed his agency to devise new ways to speed their path to patients.
“We’re at a turning point when it comes to this novel form of therapy,” he said.
If a gene therapy could reverse diabetes, the impact on human health could be huge. In the U.S. alone, diabetes afflicts roughly 30.3 million people, or 9.4% of the population.
In both types of the disease, insulin ceases to do its usual job of helping transport glucose from food to the body’s muscles and organs. In Type 1 diabetes, the immune system, for reasons unknown, attacks beta cells and crimps insulin supply. In Type 2 diabetes, beta cells die off after organs become resistant to insulin’s effects. In both cases, blood sugar reaches dangerous levels.
Having either form of the disease — especially if it is not controlled with diet, exercise and medications — raises a patient’s risk of heart disease, stroke, kidney failure, vision problems and nerve and circulatory problems in the extremities.
The World Health Organization estimates that 422 million people around the world suffered from diabetes in 2014, up from 108 million in 1980. It is on the march in some of the most populous countries, where growing affluence is shifting diets and activity patterns in ways that increase obesity, and with it Type 2 diabetes.
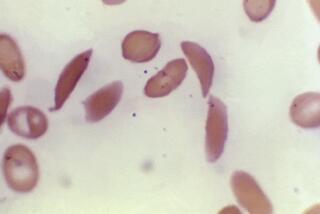
As a prospective treatment for an autoimmune disorder such as Type 1 diabetes, gene therapy could offer unique advantages. The healthy alpha cells that are induced to change their function occupy much of the same real estate in the pancreas as the beta cells. The two types of cells even look similar, and alpha cells are plentiful, so they are readily available for reprogramming.
After the defanged virus delivered the instructions for making two proteins — called Pdx1 and MafA — into the pancreas, some alpha cells began functioning like beta cells. Yet the change prompted no alarm in the immune system, since the alpha cells had been there all along.
For those with Type 1 diabetes (formerly known as juvenile diabetes because it is usually diagnosed at a young age), gene therapy could offer an alternative to existing treatments.
Currently, the only alternative to relying on a lifetime of insulin injections is to undergo a transplant of a portion of the pancreas, or of specialized islet cells from a deceased donor. While such transplants can jump-start the resumption of insulin production, patients who get them must take anti-rejection drugs for the rest of their lives. Those drugs are costly, intrusive and heighten the risk of developing infections.
Gittes and his colleagues have developed a way to deliver the therapy directly to the pancreas through a nonsurgical endoscopic procedure that is already widely performed. Once in the pancreas, the virus and its cell-altering payload appears to stay put, Gittes said, reducing the likelihood it could cause mischief elsewhere in the body.
“We’ve been excited about approaches like this,” said Andrew Rakeman, assistant vice president for research at JDRF, formerly known as the Juvenile Diabetes Research Foundation. “It has, at least theoretically, the possibility of restoring function in people whose beta cells have all been destroyed.”
Rakeman said the finding that the therapy’s effect was not permanent was “disappointing.” But, he added, “we have to take what’s reality. … Patients might need to be re-treated.”
At the same time, he said, further work by Gittes and his team may offer insights into what makes the immune system attack beta cells in the first place, and how to foil such attacks for longer periods.
Gittes said it is “quite realistic” that human clinical trials could be launched “in the immediate foreseeable future.” Those trials would be designed to test the safety and effectiveness of the experimental therapy in patients with both types of the disease, he said.
MORE IN SCIENCE
Humans may look for the helpers, but bonobos prefer the troublemakers
In the DNA of an ancient infant, scientists find traces of the very first Americans
A popular sugar additive may have fueled the spread of not one but two superbugs