A popular sugar additive may have fueled the spread of not one but two superbugs
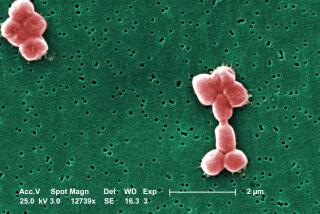
Two bacterial strains that have plagued hospitals around the country may have been at least partly fueled by a sugar additive in our food products, scientists say. Trehalose, a sugar that is added to a wide range of food products, could have allowed certain strains of Clostridium difficile to become far more virulent than they were before, a new study finds.
The results, described in the journal Nature, highlight the unintended consequences of introducing otherwise harmless additives to the food supply.
C. difficile is a nasty bacterium — infection can result in severe diarrhea and death — and numbers among the most prevalent hospital-acquired infections in the United States. According to the Centers for Disease Control and Prevention, nearly half a million people were sickened by the bug in 2011. Some 29,000 of those patients died within 30 days of being diagnosed with C. difficile, and about 15,000 of those deaths were directly linked to the infection.
The disease wasn’t always such a scourge of the sick and hospitalized, and scientists have long been trying to figure out why certain strains have become so successful in recent years. The misuse and overuse of antibiotics has long been thought to be responsible for the rise of many kinds of antibiotic-resistant “superbugs.”
To probe the mystery, a team of scientists led out of Baylor College of Medicine in Texas examined two particularly successful lineages of C. difficile, RT027 and RT078, examining what kind of carbon-rich molecules they ate. Both types, they noticed, seemed very good at using low concentrations of the sugar trehalose as a sole carbon source.
The researchers analyzed the genomes of both RT027 and RT078. While both had RNA sequences that allowed each type to take advantage of trehalose in low doses, they did so in very different ways.
C. difficile bacteria have genes that can break trehalose into glucose (a simpler, more useful sugar) and its derivatives. But a special protein called TreR blocks the microbes from metabolizing trehalose unless the concentration of trehalose in the environment is very high.
In RT027, the TreR protein is modified in a way that lowers the bar, allowing the bacteria to metabolize trehalose even in quite low concentrations.
RT078, however, is using a different mechanism to do the same thing, having picked up four genes that are used in taking up and metabolizing trehalose. (Just one of them, it turns out, was responsible for its powered-up ability to grow in small amounts of trehalose.)
“Unexpectedly, RT078 does not share the genetic alteration in TreR that is found in RT027,” Jimmy D. Ballard of the University of Oklahoma Health Sciences Center, who was not involved in the study, wrote in a commentary. Thus, “it therefore seems that two epidemic strains of C. difficile have optimized trehalose metabolism in unrelated ways.”
The researchers tested their findings in mice. If they removed a gene for trehalose metabolism in RT027, then the strain became far less virulent. And if they added trehalose to the diets of animals affected with an unaltered RT027, the mice’s risk of death shot up.
So, was the trehalose causing a bacterial population boom? Not really. The scientists found the RT027 bacterial load in the mice to be roughly the same regardless of whether they were fed this sugar. Instead, scientists think the microbes’ improved ability to metabolize the sugar meant that they also produced more C. difficile toxins — making the bacteria far more virulent.
The researchers also took fluids from the small intestines of three human study participants who were fed a typical diet and tried to grow different strains of C. difficile in it. Sure enough, RT027 responded to the trehalose in the bodily fluid, while other strains did not.
There’s another reason scientists suspect trehalose is feeding the growth of these C. difficile superbugs: Both started making their big breaks roughly around the same time, researchers said.
“Although considered an ideal sugar for use in the food industry, the use of trehalose in the United States and Europe was limited before 2000 owing to the high cost of production (approximately U.S. $700 per kilogram),” the authors pointed out. “The innovation of a novel enzymatic method for low-cost production from starch made it commercially viable as a food supplement (approximately U.S. $3 per kilogram).”
For now, this evidence doesn’t definitively prove whether trehalose helped fuel the C. difficile strains. But the findings are pretty telling and worthy of more study, Ballard said.
“Despite these concerns, the correlative findings of Collins and colleagues’ study are compelling,” he added. “It is impossible to know all the details of events surrounding the recent C. difficile epidemics, but the circumstantial and experimental evidence points to trehalose as an unexpected culprit.”
Follow @aminawrite on Twitter for more science news and “like” Los Angeles Times Science & Health on Facebook.
MORE IN SCIENCE
11 science stories we’re looking forward to in 2018
Do psychiatrists have any business talking about President Trump’s mental health?
Autism spectrum disorders appear to have stabilized among U.S. kids and teens