Drug-resistant superbugs multiplying: CDC report IDs ‘urgent threats’
Thoughtless use of antibiotic medications continues to promote the growth of drug-resistant superbugs in the U.S., threatening doctors’ ability to combat infections, according to a new report from the U.S. Centers for Disease Control and Prevention.
The 114-page publication, which was written for the general public, offered the first comprehensive picture of drug resistance in the U.S., said CDC’s director, Dr. Thomas Frieden. He said he hoped the information would encourage doctors, patients and public health officials to take action to protect what he called a “precious national resource.”
“We talk about a pre-antibiotic era and an antibiotic era,” he said Monday. “If we’re not careful, we’ll be in a post-antibiotic era. For some patients and some microbes, we’re already there.”
Bacteria can evolve rapidly to develop resistance to antimicrobial drugs. When microbes that are susceptible to drugs die off during treatment, it can create opportunities for bacteria that aren’t sensitive to the drugs to thrive. Those bacteria can then spread, and sometimes go on to share their drug-resistant genes with other bugs, which then can also spread. (The CDC report provided an antibiotic-resistance infographic illustrating how this works.)
The chain of events is probably inevitable, but scientists hope that restricting antibiotic use more tightly -- avoiding using the drugs when they really aren’t needed -- will remove opportunities for resistance to arise, slowing the process and preserving drugs’ usefulness for patients with life-threatening or difficult-to-treat infections.
It’s hard to quantify the health-related and economic effects of drug resistance, the CDC said. But the new report suggested that more than 2 million people get antibiotic-resistant infections every year, and that 23,000 die from their illnesses. The report also cited an estimate from researchers at Tufts University that drug-resistant infections could create $20 billion in excess direct costs, and $35 billion in lost productivity, every year.
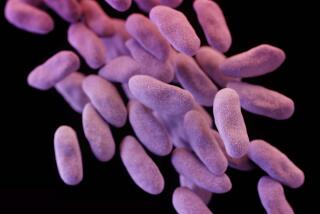
The agency identified three microbes as “urgent threats”: carbapenem-resistant Enterobacteriaceae (bacteria including some hard-or-impossible-to-treat strains of E. coli and Klebsiella, which can be deadly once they infect the bloodsteam), drug-resistant Neisseria gonorrhoeae (which causes gonorrhea) and Clostridium difficile (a bug that causes severe diarrhea, resulting in an estimated 250,000 hospitalizations and 14,000 deaths in the U.S. each year.)
C. difficile itself is not drug-resistant, but scientists attribute its spread to antibiotic use, which can wipe out beneficial bacteria in the gut, opening an opportunity for C. difficile to infect a patient.
Twelve other microbes were identified as “serious threats,” including two types of drug-resistant Salmonella, drug-resistant tuberculosis, MRSA and drug-resistant Candida (a fungus, not a bacterium.) Three more were called “concerning threats.”
The CDC report laid out four core actions for curbing drug resistance: preventing infections in the first place through immunizations, hand-washing and other precautions; tracking resistant bacteria more carefully once they emerge; using antibiotics more judiciously when needed; and promoting development of new drugs to treat -- and tests to detect -- infections.
Dr. Daniel Uslan, director of the UCLA Antimicrobial Stewardship Program, called the publication a “call to action.”
“This is for healthcare workers, it’s for pharmaceutical companies, it’s for policymakers, and it’s for patients,” he said.
Uslan oversees UCLA’s efforts to make sure its patients get the right dose of the right antibiotic for the right duration. Though California law requires that acute-care hospitals monitor antibiotic use, systems can be hard to put in place, especially in smaller hospitals with few resources, he said.
He added that he thought the largest volume of inappropriate prescriptions were handed out in outpatient settings, where many patients ask for antibiotics to treat sore throats, ear infections and other frequent woes that are often caused by viruses, not bacteria.
The CDC report also highlighted the role of antibiotic use in livestock, which often get the drugs to promote growth. In an article posted by the Natural Resources Defense Council, staff attorney Mae Wu detailed that problem, writing that almost 80% of the antibiotics sold in the U.S. are used in animals, and criticizing the Food and Drug Administration’s efforts to curb inappropriate antibiotic use in livestock thus far.