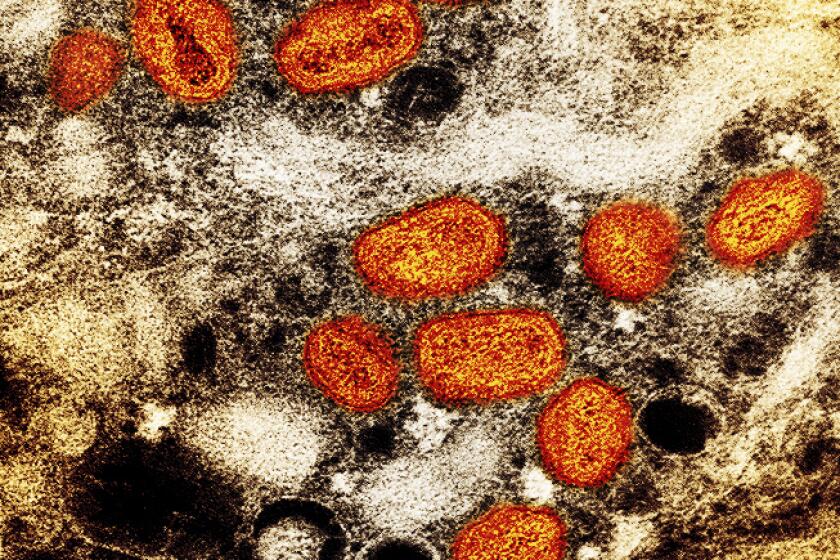
Sex, ‘casual contact,’ pimples: A California monkeypox guide, separating fact and fiction

With local, state and national officials declaring emergencies over the monkeypox outbreak and a scramble for vaccines spurring long lines — and waits — in many U.S. cities, the latest updates about the rare virus can seem overwhelming and, well, confusing.
But experts say it’s important to remember that monkeypox is a known disease that is rarely deadly (unlike the coronavirus) and already has an approved vaccine and treatment.
That’s not to say there aren’t real concerns about the outbreak, including a vaccine shortage, rapidly rising infections and the fact that one community — men who have sex with men — remains most at-risk.
The first step in addressing this virus is education, experts say, so people can better understand their risks and know how the disease spreads and how to prevent transmission.
Some are asking: ‘Would monkeypox have received a stronger response if it were not primarily affecting queer folks?’
Can only gay or bisexual men get monkeypox?
No. While the outbreak is spreading primarily among gay and bisexual men, as well as some transgender and nonbinary people, anyone — regardless of gender or sexual orientation — can become infected.
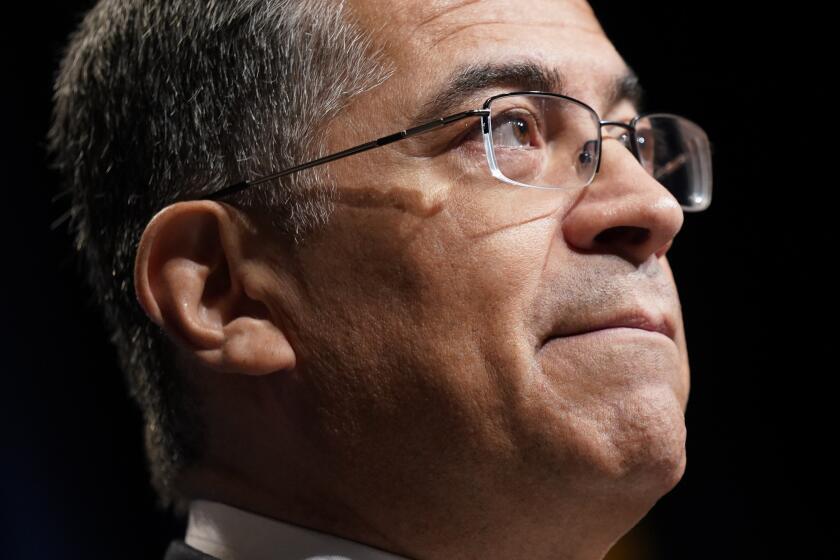
“No single individual or community is to blame for the spread of any virus,” said Dr. Tomás Aragón, California’s public health director. “Monkeypox can affect anyone, and it spreads by skin-to-skin contact, as well as from sharing items like clothing, bedding and towels.”
Dr. Stuart Burstin, the interim national director of infectious diseases for the AIDS Healthcare Foundation, said it was “by chance” that monkeypox first infected men who have sex with men. The virus has continued to spread in that group, as transmission can easily occur during sexual encounters.
Of the more than 400 confirmed and suspected monkeypox cases in Los Angeles County, 99% have been in men, about 90% of whom identified as LGBTQ, according to data from the Department of Public Health. Similar demographics from state and national health officials have found the same trend, and for that reason, gay and bisexual men, as well as some other queer people, remain most at risk.
“The risk to the general public is low, but there is a chance — and I would predict — this virus does make some inroads into the general public,” Burstin said. In very rare instances it already has: At least five children in the U.S. and one pregnant woman have been infected, according to health officials.
For decades monkeypox was not known as a disease that spreads through sex. That has changed.
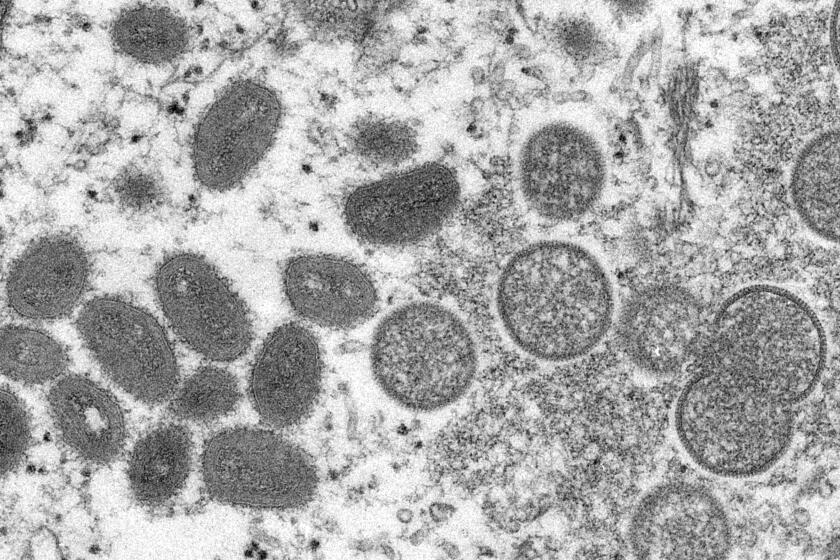
How does monkeypox spread?
Monkeypox spreads primarily through close skin-to-skin contact, but it also can be passed through infected bed sheets or towels or through “respiratory secretions,” according to the Centers for Disease Control and Prevention.
Intimate contact has to include direct, and usually prolonged, interaction with an infected sore, rash or lesion, but Burstin said such markings may not always be obvious, especially at the beginning of an infection.
“It is possible that someone can have early disease that looks like a pimple or something in the anus you can’t see,” Burstin said.
There’s no evidence that monkeypox can spread through shared airspace, like the coronavirus, experts say.
“I think it’s really important for people to recognize monkeypox is not like COVID,” Aragón said. “[Monkeypox] is very different in terms of transmission; you really have to have a close, physical contact.”
Top U.S. health officials say the country’s monkeypox outbreak can still be stopped despite rising case numbers and limited vaccine supplies.
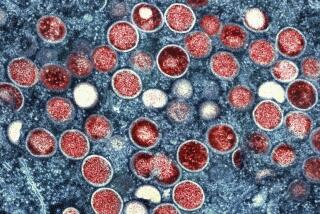
What are the typical symptoms?
Dr. Leo Moore, director of clinical services for the Los Angeles County Department of Public Health, said that people with monkeypox typically develop a flu-like illness, including fever, fatigue, muscle aches and enlarged lymph nodes. Those symptoms are then followed by a rash.
“In many instances with the current outbreak, people are developing a rash with or without swollen lymph nodes that can occur in the genital region or anally as well,” Moore said. “We’re also seeing the rash occur all over the body, including in the face.”
He said people usually develop symptoms a week or two after being exposed, but it can take up to 21 days for evidence of the virus and symptoms can last up to four weeks.
“The rash doesn’t look exactly the same on every person,” L.A. County Director of Public Health Barbara Ferrer said. That’s why it’s important to check yourself and get tested if anything looks irregular, she said.
Symptoms are usually mild, although lesions can become quite painful for some patients, Moore said. No one has died of monkeypox in California, but at least 14 people have been hospitalized for the illness.
Gay, bisexual and transgender communities fear a repeat of the AIDS-era indifference that left too many without care.
Who can get a vaccine or treatment?
The two-dose Jynneos vaccine series, which has been approved by the Food and Drug Administration for monkeypox, can be used preventatively and within two weeks of an exposure. But doses are currently limited, which has prompted health officials to set eligibility requirements so those at greatest risk of infection can get the first available shots.
In Los Angeles County, officials recently expanded eligibility, but the focus is still only on those who have been directly exposed or gay and bisexual men and transgender people who meet certain criteria, such as having multiple recent sex partners.
As for treatment, health experts say most patients can recover on their own, but there is one antiviral — tecovirimat, also known as Tpoxx — that can be administered to help ease symptoms. However, many health providers have had difficulty accessing Tpoxx, which is recommended only for use in severe cases or for people with certain high-risk health factors. CDC officials have said they are working to streamline the process so more people can get access to the drug.
As of this week, the California Public Health Department said 1,144 courses of TPOXX have been delivered and are ready for use at 71 sites around the state.
The move aims to fast-track potential new treatments and vaccines for the disease, which about 1.6 million Americans are at high risk of contracting.
Can monkeypox spread asymptomatically?
“It does not, at this point, look like there’s risk from asymptomatic spread,” said Dr. Jay Gladstein, the chief medical officer for APLA Health, an L.A. group focused on providing healthcare to the LGBTQ community.
While this outbreak continues to be studied, Gladstein said transmission has so far been linked only to contact with virus-filled lesions.
But people should know the virus can be spread until lesions have healed completely and are covered by a new layer of skin, which can take weeks.
Although the monkeypox virus can affect anyone, some gay and bisexual men are worried about being once again branded as carriers of an exotic disease.
Are massage therapists or tattoo artists at risk?
Burstin said the risk remains very low for people who work in industries that come in contact with skin, but he said it’s important to monitor for rashes or bumps.
“The safety is really very high,” Burstin said. “If you don’t see a lesion, the person is much more likely than not to not be infectious.”
He said to be extra safe, professionals should wear gloves and increase cleaning protocols, but he didn’t recommend drastically changing operations.
“The skin lesions are visible, and for the people who have them, they’re painful, so hopefully people will notice,” Gladstein said. He said there have not been any outbreaks among healthcare workers who provide care to patients with active monkeypox.
U.S. and European health officials identify a number of cases of monkeypox, an illness previously limited mostly to central and western Africa.
Should gyms, bars, swimming pools or public transportation be worrisome?
“What we’re not seeing is casual spread. It’s really got to be really close contact,” Gladstein said. “The risk is going to be vanishingly low, close to zero.”
Moore said there are certain precautions people can take in crowded spaces, such as wearing long sleeves and pants to limit skin-to-skin contact. He recommended wiping down equipment at the gym and washing your hands. But surface contact and short-term interactions are not how monkeypox is transmitted, experts say.
As for swimming pools, Burstin said he’s not worried, given the chlorine and how anything in the water would be diluted.
He said there are scenarios, such as being at a club with an event for gay men where many people could be shirtless, that he would consider more risky. But most day-to-day interactions should not concern people. He said he wouldn’t worry about brushing someone’s arm at a bar or on public transportation.
“This type of contact disease is usually not that rapidly transmitted,” Burstin said.
Everything you need to know about monkeypox.
Can using condoms prevent the spread?
Unfortunately, condoms are not a foolproof way to prevent contracting monkeypox, but they can be protective, experts say. Researchers have noticed in this outbreak that many patients’ lesions have been concentrated on genitalia or the anus — in which case a condom could provide protection — but just as many have reported infectious lesions elsewhere on the body.
“A condom is not going to be perfectly protective,” Burstin said. “That doesn’t mean people shouldn’t wear condoms; it may give some degree of protection.”
Monkeypox is not considered a sexually transmitted disease, but researchers are still trying to determine whether it can spread through semen or vaginal fluids. Some studies have indicated that possibility, so experts also recommend using a condom for a few weeks after recovering from the virus.
The appointment of a White House coordinator and deputy coordinator to deal with monkeypox mirrors the Biden administration’s response to COVID-19.
Does the smallpox vaccine provide protection?
Adults who may have received a smallpox vaccine could have some protection against monkeypox, but experts say it’s very limited.
“There’s not any significant protection as far as we know,” Gladstein said. “They may end up with a slightly more mild case of monkeypox, but it’s certainly not considered fully protective.”
As with all vaccines, he said, protection wanes over time, and with the U.S. smallpox vaccine campaign ending in the 1970s, no one should rely on that inoculation.
People who got the smallpox vaccine are eligible for the Jynneos shot.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.