Inside the Life Care Center of Kirkland nursing home, the U.S. epicenter of coronavirus

KIRKLAND, Wash. — Feeling festive, Pat McCauley looked around the crowd as she accompanied a dear friend into a Mardi Gras party at his nursing home.
A jazz band played “When the Saints Go Marching In” while a woman on staff wearing a masquerade mask strutted to the music, took photographs and handed out plates of Cajun sausage and rice.
Many residents wore jester hats that some had made the previous week.
It was Ash Wednesday, Feb. 26, and a man from a local parish had anointed some patients with ash.
McCauley was happy to see her friend and more than 30 other residents taking a break from their medical woes, although one thing struck her as odd: In the hallways, many staffers wore surgical masks.
Nobody knew it yet — though plenty of clues existed — but there was an uninvited guest at the party: the novel coronavirus.
It had been there at least a week, silently spreading among the 120 residents, 180 staff and multitudes of visitors.
Three days after the party, McCauley was listening to a Seattle radio station when she heard the words “Life Care Center of Kirkland.”
She had been following the news about the coronavirus for weeks, but until that moment, she had mainly associated it with the epidemic in China.

Now the radio station was reporting that COVID-19 had reached her leafy Seattle suburb and could be rampant at the nursing home.
Two people there — a health worker in her mid-40s and a resident in her 70s — had been hospitalized and tested positive while more than 50 others had begun to show symptoms.
Memories of the party suddenly gave McCauley chills.
She wondered if the homemade green-foam hats, festooned with gold balls, had become vectors for disease as staff members moved from resident to resident to try them on.
And what if the man from the parish had gone on to more nursing homes and touched the foreheads of other elderly, vulnerable residents?
McCauley, 79, and her husband, 80, had been visiting their friend regularly since mid-February.
How long had the deadly virus been lurking at the nursing home? Were they also infected?
::
Pat and Bob McCauley met in Dallas in 1959 as undergraduates at Southern Methodist University. She had a scholarship for academics, and he had one for swimming.
They started a family in Seattle, where he worked for Boeing, and moved from there to California and then in 1976 to Brussels for his job with a telecommunications company.
It was there that they met Neil Lawyer, a fellow American with a wife and children close in ages to the four McCauley kids. He and Bob coached flag football together.

The McCauleys kept in touch with him after moving back to Washington state in the late 1980s, learning in mid-February that he was in the nursing home blocks from their house.
An 84-year-old widower, Neil often didn’t feel well, and had memory lapses. But Pat found his Facebook page and printed photos of his children and grandchildren for an album.
One evening, Pat brought him a sweater. There was no one at the front desk, and the usual logbook to sign wasn’t there.
She found it peculiar that security and monitoring of visitors was so lax.
Still, she was impressed with all the activities available to patients.
Photocopied calendars in the lobby showed events every day — an outing to the Olive Garden restaurant, a tea party with a performance by an organist, painting with an artist.
On Friday, Feb. 21, the McCauleys wheeled Neil into a crowded room at the nursing home to see a country duo called Bob and Kevin.
The following Monday, Pat and her husband arrived at the nursing home to find that Neil had been assigned a roommate in his already cramped quarters. Ken Holstad, 73, had Parkinson’s disease and dementia.
And, they noticed, he had a cough.
When he skipped the Mardi Gras party that Wednesday, Pat brought him back a hat.
That Friday, Feb. 28, Bob walked in to the nursing home while Pat parked. A receptionist explained that visitors were now required to wear masks because of an unidentified “respiratory virus.”
The couple left immediately. When they got home, Bob was fuming. He called Seattle & King County Public Health to urge the department to investigate. The woman he reached seemed uninterested.
“Finally I told her that my last resort, if Public Health wouldn’t do anything, was to call the Seattle Times,” he wrote that day in a typed account. “She was not impressed with this either, telling me to ‘Go ahead.’”
And so he did, speaking to a reporter who said he would look into it.
The next day, Pat heard the radio report about Life Care and started making a log of her experiences at the nursing home — the party, the concert, the time she washed out a cup for Neil in the bathroom he shared with his ill roommate.
::
She and Bob decided to quarantine themselves in their house for two weeks.
They fretted about Bob’s vulnerability. He had diabetes and a heart condition, and had sustained a concussion in a recent fall.
More worrisome, on March 1 he started coughing and his body began to ache.
He wanted to be tested for the virus. But when he called Kirkland’s EvergreenHealth hospital that day to explain that he had visited Life Care several times, he was told that under federal guidelines, only people who were critically ill could get tests.
When Pat wasn’t disinfecting the house, she sat at her vintage desktop computer, searching for anything she could learn about the nursing home and its role in the outbreak.

She soon discovered that 25 Kirkland firefighters — who had responded to about 30 medical calls from Life Care in February, compared with seven the month before — had gone into quarantine.
And she read that more than a dozen nursing students at Lake Washington Institute of Technology, a public college in Kirkland, had visited Life Care the previous week.
In a series of blog posts, the school’s president explained that crews were disinfecting the campus, and that she was still trying to get guidance from public health officials on what to do about the students.
Pat was distressed that no one from Life Care or the health department seemed to be checking the nursing home’s visitor logs and calling people to advise quarantine.
When she got somebody from the nursing home on the phone on March 2, she was told not to worry because it had been five days since she visited and she had no symptoms. That was hardly reassuring. Public health authorities were recommending 14 days of quarantine for anybody who was exposed.
The same day, media reported that a total of six people in Washington state had died, all in Kirkland and three of them linked to Life Care.
And the governor of North Carolina announced the first infection there — a resident of the state who had visited Life Care.
The nursing home was now by any measure the U.S. epicenter of the epidemic.
“Instead of asking if you have traveled to China, they need to ask, ‘Have you traveled to Life Care?’” Pat said.
Washington recorded three more deaths the next day, including a Life Care resident who had been hospitalized Feb. 24.
Pat took special note of the date. It was two days before the Mardi Gras party. Surely, she thought, Life Care managers would have known that a coronavirus test was being conducted.
“We should have been told there was a respiratory virus, and they should have canceled the party,” she said.
Timothy Killian, a crisis communications specialist hired by the nursing home — part of Life Care Centers of America, the largest elderly care company in the country — said managers had acted properly, following protocols that encourage ill patients to avoid group activities and stay in their rooms.
He said that on the day of the party, staff members reported what they believed to be a flu outbreak to local public authorities.
But Brent Champaco, a spokesman for Seattle & King County Public Health, said it wasn’t until late the next day, Feb. 27, when Life Care first contacted the agency and filed notice of an “increase in respiratory illness.”
“There was nothing in the original notice from Life Care that this was an unusual type of illness, or unusual in any way or manner,” he said.
Killian said the nursing home managers didn’t learn coronavirus was present until Feb. 29 at 12:30 a.m., when they were notified of the first positive test result. It was the patient who was hospitalized on Feb. 24 and later died.
He said the company did not learn until after Feb. 29 that coronavirus had been in the building since at least Feb. 19 — the hospital admission date for another patient who turned out to be infected.
Given the urgent needs of the patients, notifying visitors about possible exposure to the virus was not a priority, Killian said.
The McCauleys had grown livid.
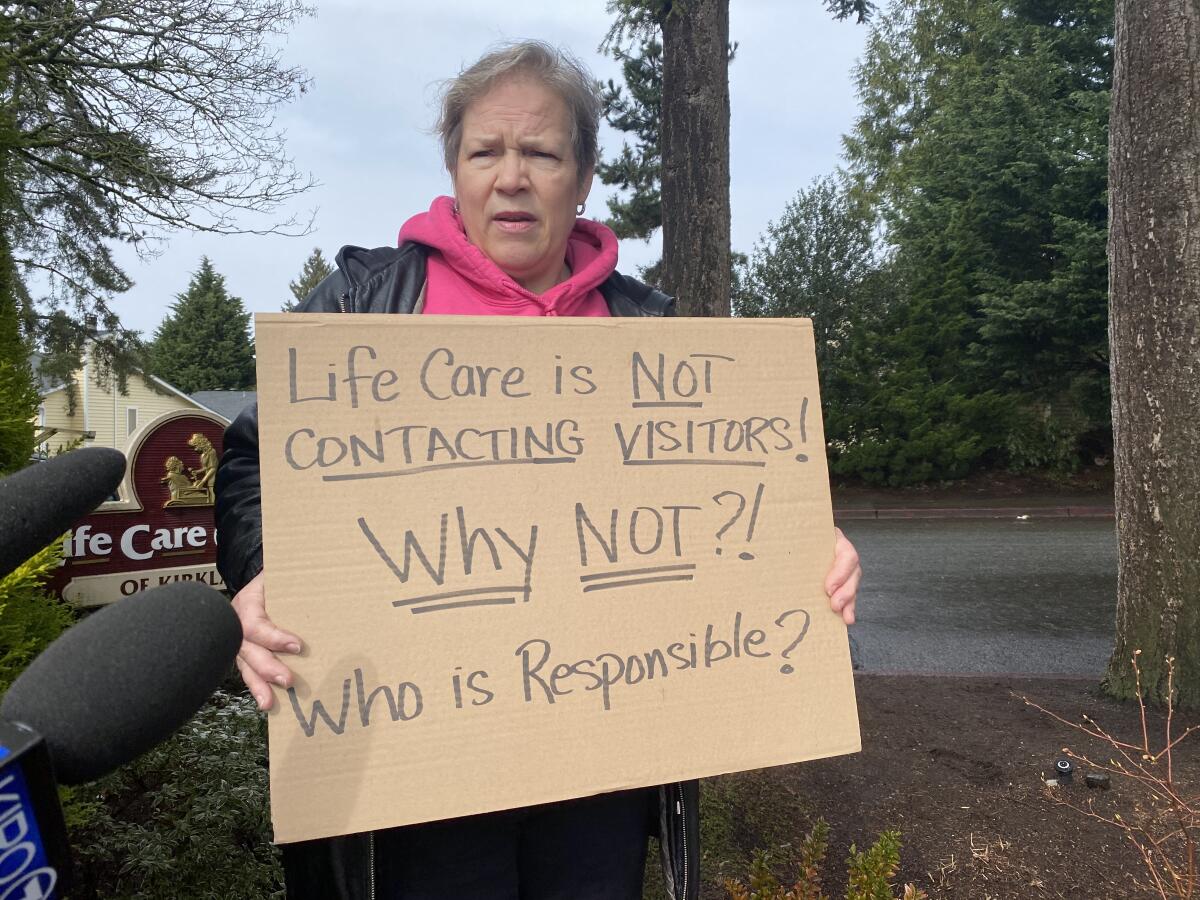
At Killian’s first news conference on March 7, their youngest daughter, Cheri Chandler, stood behind a battery of television cameras holding a cardboard sign.
“Life Care is not contacting visitors!” it said. “Why not? Who is responsible?”
Pat was still digesting the news she had received that morning: The previous day, Neil had been rushed to an isolation room at EvergreenHealth.
That evening, she said, he tested positive.
::
It felt like the virus was closing in on Pat and her husband.
On March 8, Pat felt feverish and took her temperature. It was just above normal at 99 degrees.
She received a call that day from a doctor named Eric Chow, of the U.S. Centers for Disease Control and Prevention. He had gotten her name not from Life Care or local public health officials, but from one of their friend’s sons.
Chow said that Pat and Bob should be tested for the virus.
They were wise to have stayed in their home, but also needed to isolate themselves from each other by sleeping in separate beds, using different bathrooms and wearing face masks, he said.
The couple arranged for tests nearby at Overlake Medical Center — the only time they broke their quarantine. A doctor in what resembled a spacesuit and helmet inserted a swab deep into Pat’s left nostril and twisted it while counting to six. The same for Bob.
They returned home and went to their separate rooms. The next day, March 9, at 4:30 a.m., Pat’s phone rang.
Neil was dead.
It had happened the previous evening, his daughter explained.
Later, Pat learned about the surreal scene at his deathbed. Each family member who entered his room had to go alone, in full protective gear. There could be no embrace, no caress.
Pat’s grief deepened at the thought of parting with a parent in such a way. The virus that isolated her from her family, friends and community — even from her husband, within their own home — ensured that its victims died alone.
As the McCauleys anxiously awaited their test results, their daughter dropped food and supplies at their doorstep, sometimes waving at them though a window.
She spent $180 on Amazon for two packets of Cold-Eeze zinc lozenges. A brother on a business trip in Mexico found N95 respirator masks to send.
On March 10, health officials released a list of nine more Washington nursing homes with coronavirus infections. Pat wondered again about where the parish representative had been.
The same day, Neil’s roommate, Ken, was admitted to a Seattle hospital after testing positive for COVID-19. A relative in his 50s who had visited him also became ill with the disease.
Pat’s low-grade fever persisted. Bob’s cough had worsened and kept him awake at night. Finally on Thursday, they received a call.
Both tests were negative, a doctor said. But she said that tests were generating many false negative results. They should stay in quarantine, and might need tests again.
As of Saturday, the official death toll at Life Care was 27 — nearly half the U.S. total of 57.
“Sadly you can’t depend on the agencies that are supposed to be protecting you,” Pat said. “If somebody had gone in sooner, maybe there wouldn’t have been so many deaths.”
From her kitchen window, she watches the flashing red lights of emergency vehicles converging on the nursing home.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.











