The CDC is changing the way it monitors COVID-19 in the U.S.

Acknowledging that it is losing some of its eyes and ears across the United States, the Centers for Disease Control and Prevention this week unveiled a scaled-down COVID-19 surveillance system for the post-pandemic era.
The CDC’s new monitoring network won’t have the fine resolution on the coronavirus that the agency strove for during earlier stages of the pandemic. But it will lash together a raft of new and existing tools to keep an eye on the virus while also keeping broader tabs on the public’s health.
With the federal government’s three-year-old public health emergency set to expire next Thursday, the agency will begin to track COVID-19 cases alongside other respiratory illnesses, said Dr. Nirav D. Shah, the CDC’s principal deputy director. New cases of the pandemic virus, which has caused 1.1 million deaths in the United States and 6.9 million deaths worldwide, will eventually be lumped together with influenza, respiratory syncytial virus and other infections that can cause pneumonia and death in humans.
The CDC will still be able to alert communities to upticks in coronavirus spread based on its continued tracking of emergency department visits, COVID-19 hospitalizations and wastewater surveillance from local sewage plants. Reliable statistics on COVID-19 deaths will lag behind other data.
The COVID-19 death rate in the U.S. fell by nearly 50% in 2022, a decline credited to widespread vaccinations as well as a rise in natural immunity.
Shah said the CDC’s plan will yield a picture of the pandemic virus that is “superior” to the data it gathers on flu and RSV. However, the agency’s website will no longer offer detailed insights on local conditions that many Americans had come to rely on. And the data that will be posted will be collected and updated less frequently.
“CDC will continue to closely monitor COVID-19 and provide the information to which we have access,” Dr. Rochelle Walensky, the agency’s outgoing director, told members of the U.S. Senate Committee on Health, Education, Labor and Pensions on Thursday. “We have worked hard to sustain the data to understand what’s happening with the virus in America. But the end of the [public health emergency] means the CDC will no longer be able to collect data and share information many Americans have come to expect.”
For instance, the CDC’s color-coded COVID-19 community risk maps, which have provided county-level assessments of coronavirus spread, and of local hospitals’ capacity to care for infected patients, will be discontinued, Shah said.
Adopted in February 2022, the CDC’s COVID-19 Community Level maps relied heavily on Americans’ willingness to get tested at labs and clinics, which in turn reported numbers and rates of new infections to the agency. But milder infections have prompted less testing and at-home testing has become the norm — trends that have dried up the CDC’s sources of reliable localized data.
Indeed, in recent months, experts have concluded that the CDC’s count of new cases is no longer a reliable measure of the coronavirus’ spread.
The WHO said that even though the emergency phase of COVID-19 is over, the pandemic hasn’t come to an end, noting recent spikes in cases in some regions.
At the same time, many states and counties have stopped gathering or reporting COVID-19 data altogether. That has added to the difficulty of maintaining and updating local risk maps and of documenting health disparities based on race and ethnicity, Walensky said.
The CDC will also lose some insight into the demographics of people seeking vaccines. Most, though not all, states and territories have pledged to continue to share the age, gender and ethnicity of people being vaccinated for COVID-19. But those details will no longer be updated regularly on the CDC website.
“We will make do,” Walensky said on Capitol Hill. “However, this should worry us all, primarily because what it says about the visibility we will have into the next outbreak. We will be back to square one.”
To monitor the virus that causes COVID-19, the CDC will rely on an established network of healthcare systems and public health departments across the country that already help the agency monitor respiratory and other illnesses. They will supply real-time data on patients being treated for COVID-19 and other flu-like illnesses, and the CDC will comb through death certificates for information about COVID-19 fatalities.
Surveillance networks such as RESP-NET, meanwhile, will continue to collect lab data on respiratory viruses from regions that cover more than 29 million people in 13 states. A second system of 450 labs across the nation will provide the CDC with data on viruses that cause respiratory ailments.
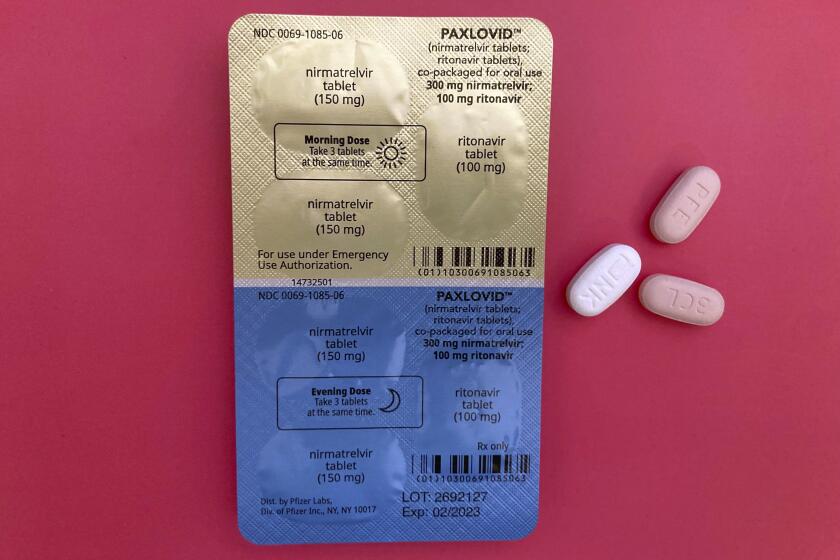
A pandemic allows the Food and Drug Administration to authorize vaccines and drugs for emergency use, even after the health emergency ends.
Over the past two years, the agency has recruited and trained a growing cadre of partners — local health departments, wastewater treatment plant managers and private and academic labs — to help it detect, sample and measure concentrations of the SARS-CoV-2 virus in sewage. Shah said that new network will continue to assess the water we flush down our toilets and send down our drains to provide early warning of worrisome trends.
Wastewater surveillance can provide highly local evidence that infections have ticked upward, even if the people shedding the virus have not been diagnosed. The data are especially useful if followed by a hike in COVID-19 hospitalizations, and they can be combined to paint a national picture of the rise and fall of infections. (Wastewater surveillance also helped detect the spread of mpox in Los Angeles and has signaled the presence of antibiotic-resistant strains of bacteria in the county as well.)
Combined with genetic sequencing — another public health tool that has come into wide use during the pandemic — samples taken from wastewater can help detect changes in the pandemic virus, including the emergence of new variants.
A new program of gathering and genetically sequencing biological samples from travelers — voluntarily as well as from the wastewater of commercial aircraft — is expected to lend insight into coronavirus variants entering the United States from abroad.
Using machine learning, scientists have trained computers to comb the internet and recognize the early signs of a COVID-19 surge up to 6 weeks in advance.
Dr. Brendan Jackson, the CDC’s COVID-19 response manager, said genetic sequencing would remain one of the public health agency’s sharpest tools, both to detect potentially dangerous mutations in the virus as well as recombinations that could change its behavior altogether.
Shah expressed confidence that given the wide range of data sources it will continue to have, “we will have good sight lines” into the state of COVID-19 in America.
“We will still be able to tell that it’s snowing even though we will not be able to count every snowflake,” he said.
Times staff writer Karen Kaplan contributed to this report.