When it comes to preventing COVID-19 deaths, ‘how we feel about each other matters’

The United States has the dubious distinction of suffering the highest COVID-19 mortality rate among the world’s high-income countries. But that national average — 372 deaths per 100,000 people as of last summer — hides the fact that pandemic outcomes differed greatly from state to state.
In a comparison that controlled for demographic differences between states, Arizona’s COVID-19 mortality rate of 581 deaths per 100,000 residents was almost four times higher than Hawaii’s, where there were 147 deaths per 100,000 residents. Death rates in the hardest-hit U.S. states resembled those of countries with no healthcare infrastructure whatever. States that fared best had rates on a par with countries such as Australia, New Zealand and South Korea, which worked zealously to keep their pandemic death tolls low.
What accounts for these wide disparities? A new study offers some intriguing answers.
Race, ethnicity and socioeconomic factors were the most powerful predictors of a state’s COVID-19 death toll, researchers found. The larger the proportion of residents who identified as Black or Latino, the higher the poverty rate, the greater the share of residents without health insurance and the lower the education level among adults, the more deaths there were per capita.
That may not be much of a surprise. But the researchers also discovered that the more people in a state trusted one another, the lower their collective risk of dying of COVID-19. That result underscores how America’s growing divisiveness seems to have made us uniquely vulnerable during the pandemic.
“How we feel about one another matters,” said political scientist Thomas J. Bollyke, one of the study’s lead authors. “The solidarity between people — the feeling that others will also do the right thing, that you’re not being taking advantage of — is a big driver in your willingness to adopt protective behaviors.”
California is set for a full reopening on June 15, but experts say a full recovery is dependent on trust.
The report, published last week in the medical journal Lancet, is based on troves of U.S. pandemic data from January 2020 to July 2022. Bollyke called the undertaking “the most comprehensive statement to date on the drivers of outcomes in the pandemic.”
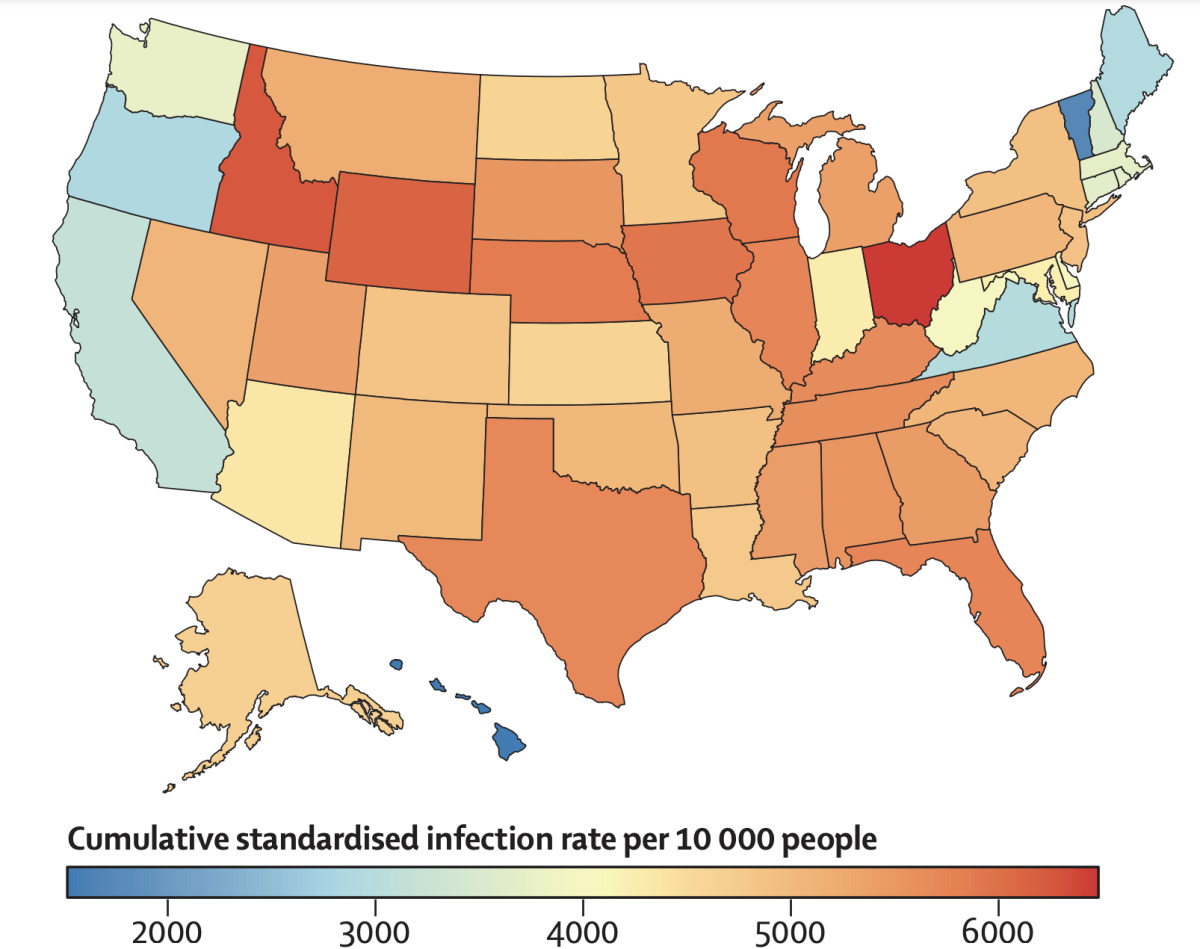
Scores of researchers from across the country extracted data on states’ demographic characteristics prior to the pandemic, looking for ways in which their behaviors and policies diverged as the pandemic proceeded. To make direct comparisons between states, they created standardized measures of infection and death rates that accounted for differences in COVID-relevant factors such as the ages and underlying health conditions of residents.
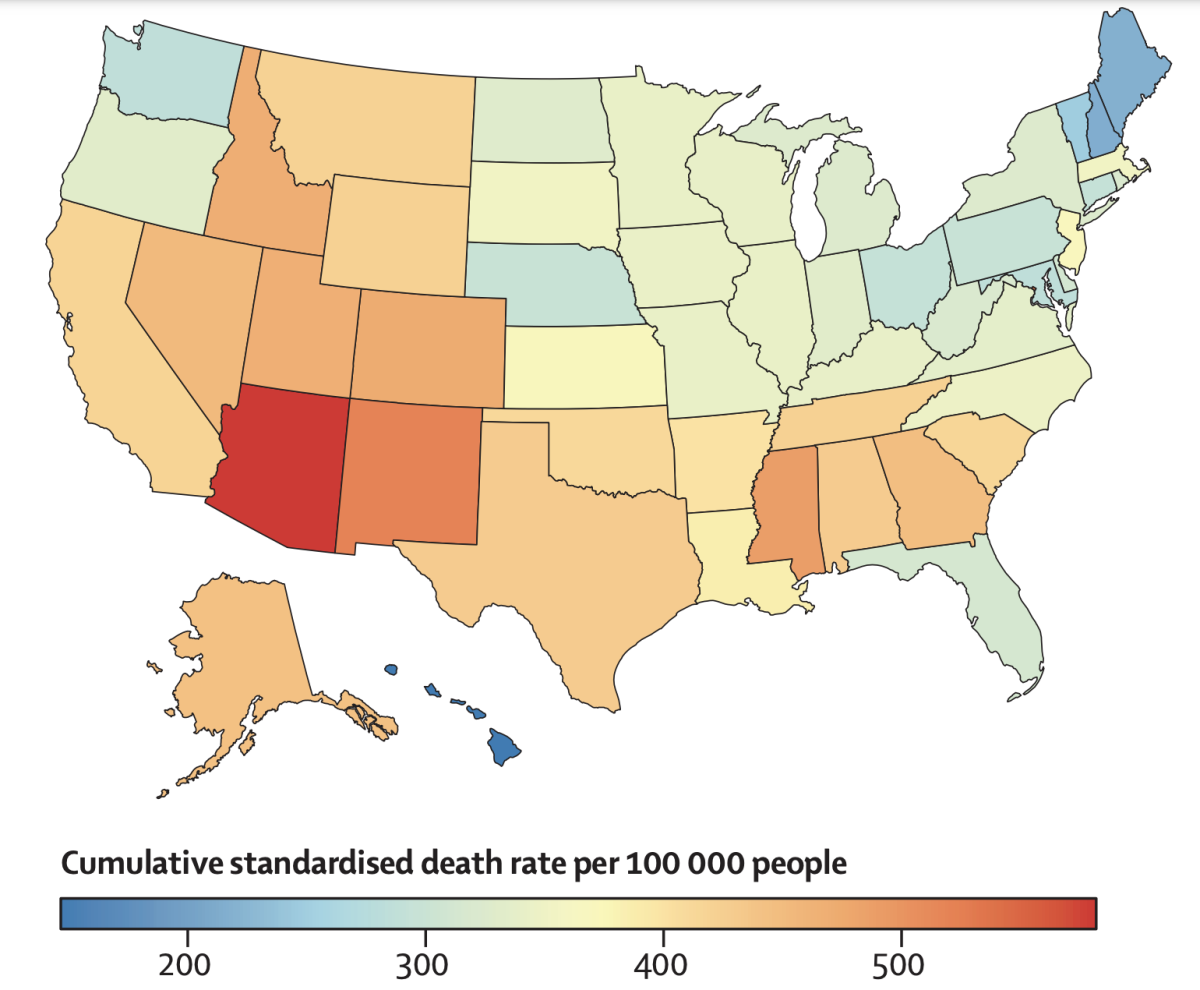
For instance, California’s unadjusted rate of 291 COVID-19 deaths per 100,000 residents was lower than all but 11 states. But once research factored in that the state has a relatively young population with a low prevalence of conditions that make people vulnerable to severe cases of COVID-19, the mortality rate rose to 418 deaths per 100,000 residents. Only 15 states fared worse, the study authors found.
Demographics told only part of the story. Policy decisions mattered too.
Most states adopted some kind of masking and social distancing mandates early in the pandemic, but there was wide variation on how stringent they were and how long they lasted. When the researchers assigned each state a “mandate propensity,” they found that states that scored high in their imposition of public health measures had lower coronavirus infection rates.
California had the highest mandate propensity, while Oklahoma had the lowest. The researchers calculated that if Oklahoma had embraced masking and social distancing restrictions to the same degree as California, Oklahoma would have seen 32% fewer coronavirus infections.
However, more aggressive public health mandates did not translate into lower mortality rates. The authors surmise that is probably explained by the fact that many older and sicker people, who were most likely to die if infected, took steps to protect themselves whether or not their state governments issued strict rules.
The White House is defending President Biden’s order that federal employees get vaccinated against COVID-19 after a federal appeals court blocked it.
The researchers also found that a state’s mandate propensity had no bearing on the health of its economy, as measured by its gross domestic product. States with less mask use and fewer restaurant closures did have higher employment levels, but that extra economic activity came at a price: Each percentage-point increase in a state’s employment was associated with 143 additional deaths per 100,000 residents.
No single factor was more important than “vaccinated person days” — a measure of how much of a state’s population was vaccinated, and how early. If Alabama, which had the lowest score on that measure, had achieved the vaccine coverage seen in Vermont, the highest-ranking state, it would have seen 30% fewer infections and 35% COVID-19 deaths during the study period, the researchers estimated.
Another notable finding: Vaccination mandates for state employees, which prompted many legal challenges, “stood out” for their association with lower infections and fewer deaths, the authors wrote.
The study highlights the tangible toll of the country’s us-versus-them mentality, which was on full display during debates over masking in schools and vaccine mandates for government employees. We don’t trust one another very much, which makes us less willing to do things to protect one another.
“Interpersonal trust” has been measured since the 1950s, and levels of that positive feeling toward others have declined steeply in the United States since the early 1990s, said Bollyke, who directs the Global Health Program at the Council on Foreign Relations. That trend has been driven by a decline in economic conditions for lower-income people with college degrees. It’s particularly low among Black Americans, and among those who voted for Donald Trump in the 2020 election.
Trust in the federal government and trust in science did not register as major drivers of COVID-19 death rates. But trust in fellow citizens held up strongly, Bollyke said.
Trust is key as we reopen with the coronavirus still present
The associations the study uncovered clearly suggest that the strengths and weaknesses that states take into a national emergency — and some of the policies they adopt to respond to a crisis — make a big difference, said Lawrence Gostin, an expert in public health law at Georgetown University.
“This is a strong vindication of states that took COVID seriously, that used science and that mitigated health inequalities,” Gostin said. “A lot of the political rhetoric — that mandates don’t work, and that equity is not important — was just proven wrong.”
The study’s findings can be put to use to save lives long before the next pandemic, said Dr. Steven Woolf, a researcher at Virginia Commonwealth University who tracks the health status of Americans.
“Many of the same factors are affecting health outcomes right now,” Woolf said.