Could a homegrown coronavirus strain be partly to blame for California’s surge?
California scientists have discovered a homegrown coronavirus strain that appears to be propagating faster than any other variant on the loose in the Golden State.
Two independent research groups said they stumbled upon the new strain while looking for signs that a highly transmissible variant from the United Kingdom had established itself here. Instead, they found a new branch of the virus’ family tree — one whose sudden rise and distinctive mutations have made it a prime suspect in California’s vicious holiday surge.
As they pored over genetic sequencing data in late December and early January, the two teams saw evidence of the new strain’s prolific spread leap off their spreadsheets. Though focused on different regions of the state, they uncovered trends that were both remarkably similar and deeply worrying.
Researchers at Cedars-Sinai Medical Center in Los Angeles found that although the strain had been barely detectable in early October, it accounted for 24% of roughly 4,500 viral samples gathered throughout California in the last weeks of 2020.
In a separate analysis of 332 virus samples culled mostly from Northern California during late November and December, 25% were of the same type.
“There was a homegrown variant under our noses,” said Dr. Charles Chiu, a laboratory medicine specialist at UC San Francisco who examined the samples from the northern part of the state with collaborators from the California Department of Public Health. Were they not on the hunt for the U.K. strain and other viral variants, he said, “we could have missed this at every level.”
British scientists have bolstered their case that the new coronavirus variant spreads more easily than its predecessors. It could be worse in the U.S., they warn.
The new strain, which scientists have dubbed B.1.426, bears five mutations in its genetic code. One of them, known as L452R, alters the virus’ spike protein, the tool it uses to infiltrate human cells and turn them into virus-making factories.
Over multiple generations, even a small improvement in this ability will help a virus propagate more easily through a population, driving up infections, hospitalizations and deaths.
Spotty surveillance efforts that use genetic sequencing to track changes in the virus had detected a single instance of B.1.426 in California way back in July. As far as scientists can tell, it lay low for the next three months.
Then it got busy.
The team at Cedars-Sinai collected 192 viral samples from patients at the medical center between Nov. 22 and Dec. 28. At 11 p.m. on New Year’s Eve, they uploaded those samples to their genetic sequencer, which began to spit out the data over the first weekend of the new year. The strain’s sudden prominence elicited both wonder and sorrow.
“We said, ‘Wow! There’s something different, something we didn’t expect to find,’” said Dr. Eric Vail, a pathologist who usually sequences genes in search of cancer drivers. “All of a sudden, your brain starts going a mile a minute.”
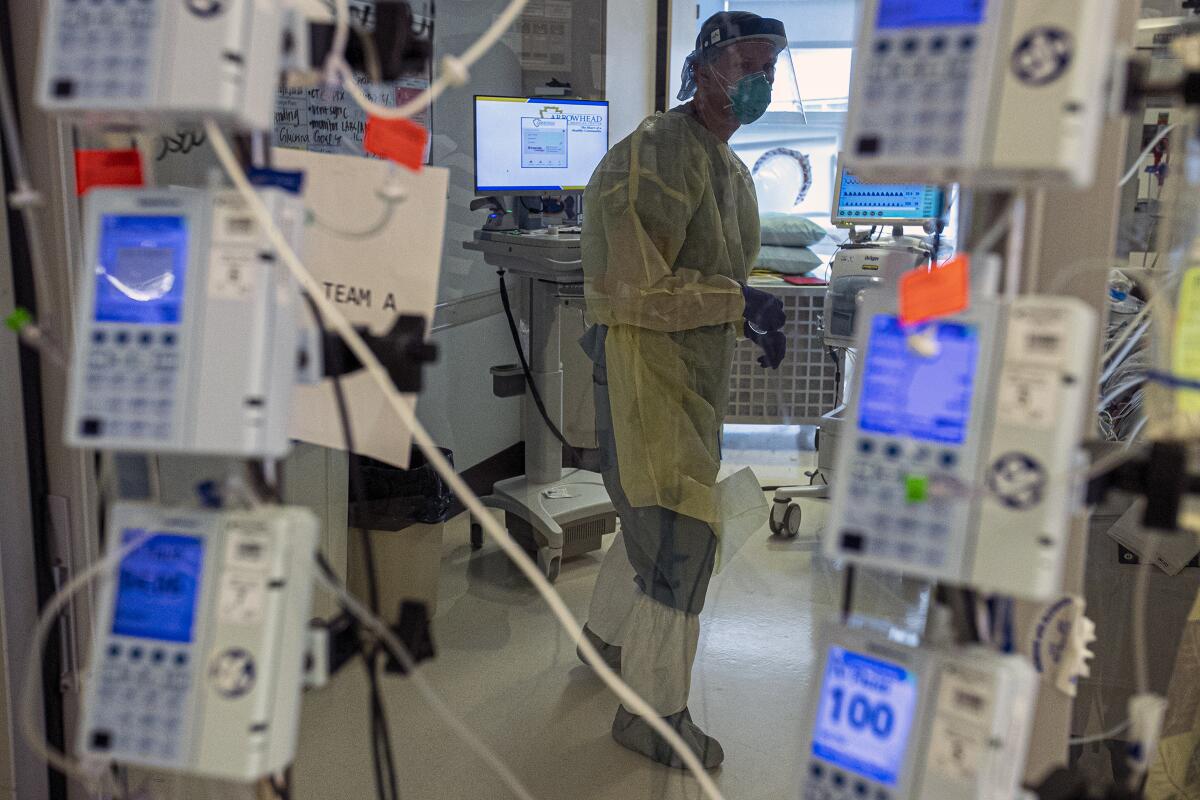
All thoughts quickly turned to the state’s calamitous COVID-19 surge — a run-up in illness and death that stressed hospitals to their limit, killed more than 18,000 Californians and doubled the state’s total death toll in the space of less than three months.
Had they found the culprit?
The preliminary evidence seemed damning. It was certainly found at the scene of the crime. Flummoxed health officials working to contain the outbreak had hypothesized that they were up against a new coronavirus strain with enhanced transmission capabilities.
But there were several other suspects to consider as well, including chilly weather, restaurant dining, holiday gatherings and a growing disregard for public health measures.
Experts say California’s brutal winter COVID-19 surge is largely driven by complacency on masking and distancing. One calls it ‘COVID resentment.’
To clarify B.1.426’s role in the surge, investigators will need to determine just how much devastation it is capable of producing. That inquiry will focus on its transmissibility as well as its ability to circumvent the tools — including masks, drugs and vaccines — that can be used to bring the pandemic under control.
For now, both sets of researchers doubt they have found a lone actor. But they may have caught an accomplice.
Chiu said his skepticism stems in part from the fact that the surge in cases across the state seems to have begun before the new strain saw its steepest growth. “It may have contributed to this surge, or simply gone along for the ride,” he said.
In addition, the strain’s sudden prominence among viral samples in Northern California could be due in part to its role in an unusually large outbreak at Kaiser Permanente San Jose Medical Center that infected at least 77 staffers and 15 patients, and resulted in one employee death. Officials are investigating whether an infected but asymptomatic employee was able to spread the virus widely with the help of a battery-powered fan that was part of an inflatable Christmas tree costume.
“It seemed to spread quite fast,” said Dr. Sara Cody, the health officer for Santa Clara County, where the hospital is located. “We are trying to understand whether the features of that outbreak are because of this variant — does this variant of the virus behave in some different way — or does it have to do with other factors that were present at the hospital?”
In Southern California, where the timelines of the surge and B.1.426’s emergence seem better aligned, researchers are more inclined to blame the virus.
“It probably helped to accelerate the number of cases around the holiday season,” Vail said. “But human behavior is the predominant factor in the spread of a virus, and the fact that it happened when the weather became colder and in the midst of the holidays when people gather is not an accident.”
Health officials set aside carefully considered plans for rolling out COVID-19 vaccines and made the shots widely available. That may hasten the pandemic’s end.
Scientists in Chiu’s lab have already begun cultivating armies of the new strain, derived from four patients recently infected with it. Creating large batches under controlled conditions is a first step in testing whether the any of its mutations enhance its ability to latch onto, invade and hijack human cells.
Those early efforts have raised cause for concern.
“It grows pretty robustly,” Chiu said.
Adding to his concern are the findings of other researchers at Howard University who engineered and tested a version of the coronavirus with the L452R mutation, which rose to prominence in a strain that surfaced in Denmark in March. The Howard team found that the mutation helps the virus attach more firmly to human cells, potentially enhancing its transmission.
In Chiu’s lab, as well as at Cedars-Sinai, scientists will put the new strain through its paces to look for signs that B.1.426’s mutations have enhanced its performance.
Other experiments will explore whether the antibodies generated by the immune systems of people who have been infected by or vaccinated against the coronavirus will recognize this new strain.
Some damning evidence has already come to light. State health officials reported this week that a patient in Monterey County who had tested positive for an infection in April and recovered has now been infected with B.1.426.
That suggests that the new strain may be able to hide its presence from antibodies created after exposure to other versions of the virus — a phenomenon known as “immune escape.” If that’s the case, it might undermine the effectiveness of COVID-19 vaccines and antibody-based treatments.
“The takeaway is that this is a variant that’s becoming more prevalent and we need to lean in and understand more about it,” Cody said.











