Q&A: Superbug: What it is, how it spreads, what you can do
CRE superbugs are becoming more widespread in hospitals and other healthcare facilities. They can cause infections that are difficult -- or sometimes impossible -- to treat. At least seven patients at UCLA’s Ronald Reagan Medical Center have been sickened with CRE infections in recent weeks, and two have died.
Here’s what you need to know about CRE.
What is CRE?
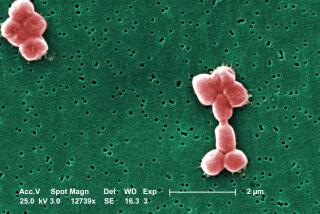
CRE stands for carbapenem-resistant Enterobacteriaceae and comprises a family of supergerms that have become immune to modern medicine’s most powerful class of antibiotics, called carbapenems. Examples of CRE bacteria include Klebsiella pneumoniae and Escherichia coli.
Dr. Tom Frieden, director of the U.S. Centers for Disease Control and Prevention, has called CRE “nightmare bacteria.”
How do I get a CRE infection?
Healthy people normally don’t get it, according to the CDC. It primarily affects hospital patients and residents of nursing homes. Those at highest risk include patients who are receiving serious medical care and have been exposed to equipment like breathing machines, catheters or IVs, as well as long-term antibiotics.
About 18% of long-term acute care hospitals and about 4% of short-stay hospitals in the U.S. had at least one CRE infection during the first half of 2012, according to the CDC.
Can CRE spread from person to person?
Yes, especially in healthcare settings. A single type of CRE has spread from one healthcare facility to at least 42 states over the past decade, according to CDC investigators.
Infected patients may have the bacteria on their hands and skin, and they shed it through urine, feces and wounds, according to the West Virginia Bureau for Public Health. Patients are likely to contaminate “doorknobs, bedrails, light switches, toilets, bedpans, bedside commodes, and bathroom fixtures,” the bureau warns, and then the infection can spread to others. The situation becomes worse if CRE hitches a ride on a blood pressure cuff or other piece of equipment that travels from room to room.
In addition, the superbugs can be transmitted by healthcare workers who fail to properly scrub their hands between patients or who don’t wear gloves and gowns when seeing patients who are infected. CRE can also spread through the use of contaminated medical devices such as ventilators or urinary catheters that are not adequately sterilized.
“If they have a medical device that gets around some of the normal body barriers, the bacteria can be introduced into a place where it normally wouldn’t be,” said Dr. Stephen Calderwood, president of the Infectious Diseases Society of America. Simple devices like catheters are easier to clean than more complicated devices with many holes in them, he added.
How dangerous is it?
If the infection spreads to the bloodstream, CRE can kill up to 50% of its patients, according to one report. Others say the fatality rate is closer to 40%. Calderwood said scientists do not have good data on so-called attributable mortality -- cases where death is known to have resulted directly from CRE infection.
Many types of bacteria in the Enterobacteriaceae family exist peacefully in the digestive system of humans, and CRE microbes usually colonize the gastrointestinal tract first. But they can cause major problems when they enter the bloodstream, the lungs, the urinary tract or other parts of the body. And once they get where they don’t belong, CRE can spread their antibiotic resistance to other kinds of germs.
Is CRE infection common?
A 2013 CDC report on superbugs estimated that CRE causes about 9,000 infections in the U.S. each year. That report labeled CRE an “urgent” threat, said Dr. Stephen Calderwood, president of the Infectious Diseases Society of America.
A 2012 CRE prevalence survey conducted by the California Department of Public Health found that while there was an overall low prevalence of CRE in California, compared to other parts of the nation, there was a higher prevalence in long-term acute care facilities and geographically in Southern California.
Nationally, states in the Northeast have the most cases of CRE, according to the CDC.
How can you tell if someone is infected with CRE?
Patients with an active infection may appear to be sick. But people who are merely hosting the bacteria in their intestines would show no outward signs, according to the West Virginia health authorities.
Hospitals face a serious challenge in diagnosing CRE infections quickly enough to keep them from spreading, Calderwood said. If an infection is suspected, workers must confirm it by growing bacteria samples and testing their sensitivity to various antibiotics -- a process that can take a day or two. Scientists are working on rapid diagnostic tests, but they are not yet available, he said.
What can I do about it?
According to the CDC, patients can help limit the spread of CRE infections by telling their doctor if they have been hospitalized in another facility or country; by taking antibiotics only as prescribed and by insisting that everyone who touches them washes their hands first.
EXCLUSIVE: 179 UCLA patients may have been exposed to deadly bacteria
Times editor Karen Kaplan contributed to this report.
“Like” Los Angeles Times Science & Health on Facebook for more medical news.