Op-Ed: My postpartum depression was not hard to predict — yet no one warned me

Being pregnant and middle-aged is like driving an old car with bald tires and worn-out brakes up a rocky mountain. In the rain. Frankly, it’ll be a miracle if you get to the top. I almost didn’t.
I was 48 years old when my daughter was born. Her birth was the culmination of a brutal, seven-year odyssey of fertility treatments. After 11 failed rounds of in vitro fertilization, one of which ended in miscarriage, I finally got pregnant using a donor egg and carried the baby to term.
My postpartum depression was not hard to predict. I had eight risk factors — advanced maternal age, use of fertility treatments, pregnancy complications, traumatic birth, history of anxiety and depression, lack of sleep, insufficient support, difficulty breastfeeding. My symptoms checked off a lot of boxes.
I wish someone had warned me. Even though there have been some recent improvements, particularly in California, in how postpartum depression is diagnosed and treated, no doctor mentioned it to me before my daughter’s birth — not my obstetrician-gynecologist, not the perinatologist, not even my psychiatrist.
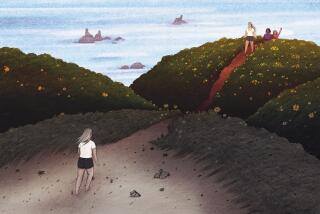
The first time I held my daughter, instead of feeling boundless joy and radiant love as I’d expected, I was overwhelmed with fear and remorse. I had the sense I was drowning in mud, holding her over my head. I thought for sure we’d both go under. Once we got home with the baby, I was so overwhelmed with obsessive anxiety that I couldn’t properly care for her.
In the first few weeks the situation devolved. An irrational fear that the baby would stop breathing and die if I looked away for more than a moment kept me from sleeping. Stress dried up my milk supply. The baby was not gaining weight, and she had blood in her stool. I feared where my escalating despair would lead.
Nationally, about 500,000 American mothers experience symptoms of postpartum depression per year, according to research from the Centers for Disease Control and Prevention. That number is rising. A recent Blue Cross Blue Shield report stated that the number of women diagnosed with postpartum depression increased by nearly 30% between 2014 and 2018. And a worldwide study published in April showed a large increase in the number of pregnant and postpartum women with significantly elevated symptoms of mental health distress during the COVID-19 pandemic.
Experts say more women are seeking out help since the pandemic began. Women of color are among the most affected, in part because of insurance issues.
Women over age 40 are having their first babies at twice the rate they did in 1990. Meanwhile, fertility rates for men and women are plummeting. Women most often delay childbirth due to costs — child-care, education and healthcare expenses have risen more quickly than wages. But the older a woman gets, the more likely she’ll need fertility treatments to conceive and, as her age increases, so does her risk for postpartum depression.
The accessibility and cost of maternal mental health care are barriers to diagnosis and treatment for many new mothers, as is the stigma of admitting you’re having trouble caring for your child.
I was lucky. I was already under the care of a psychiatrist, and my postpartum depression was diagnosed four weeks after I gave birth. I got excellent treatment in an outpatient program at UCLA that specializes in maternal mental health. I spent six hours a day, five days a week, in group therapy there, alongside six other clinically depressed mothers. Our babies attended with us.
My fellow patients and I came from different ethnic and economic backgrounds, but our symptoms overlapped. We all blamed ourselves for being ill. We felt we were failing our babies. But as time passed, we learned how postpartum depression lies. The truth was that our hormones had failed us, as had the doctors who hadn’t warned us of the symptoms of postpartum depression or diagnosed some of us when those symptoms appeared.
The cultural landscape failed us too, presenting us with unrealistic fantasies of motherhood that could be reached by following the advice of “breast is best” campaigns, milestone measuring and preening mommy blogs. We’d bought into these unreasonable expectations but were laid low by the very real challenges of parenting while managing our mental health.
In the clinic’s group therapy room the other mothers and I listened to one another’s stories and reflected one another’s experiences. Feeling compassion for them taught me compassion for myself. Their courage gave me courage. Together, over time, we healed.
There’s good news. Postpartum depression is more openly discussed in the media, and perinatal mental health screening is becoming more common. A 2019 California law requires that postpartum depression screenings be offered to all new mothers. And studies continue to be done that research the best types of treatment — in my case I found group therapy particularly effective.
But there is still a severe lack of specialized treatment, and much of what is available is not accessible to those without financial resources or good insurance. The program I attended in 2018 was one of 12 like it in the U.S. Now there are 24, but many, many more are needed. After the implementation of California’s 2019 screening law, the program I attended became so overwhelmed with women calling to join, it had to close its wait list.
All mothers with postpartum depression deserve quality treatment. The number of programs specializing in postpartum depression needs to be dramatically increased and made accessible and affordable. The stigma attached to postpartum depression needs to be erased, so that women don’t feel ashamed for seeking treatment.
Having waited so long to have a child, if my daughter starts her own family I may not be here to help her. But I can help now, by doing my best to ensure that she’ll have access to the care she may need, when that time comes.
Devorah Herbert is an Emmy-nominated production designer living in Los Angeles with her husband and 3-year-old daughter. @devherbert
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.