Robert Edwards dies at 87; Nobel winner for first ‘test-tube baby’
About 10% of married couples suffer from infertility – the inability to conceive a child naturally. Through the better part of the 20th century, physicians considered this a minor and perhaps irrelevant problem, one that contributed overall to society by keeping the birthrate down.
British biologist Robert Edwards thought differently. He was among the first to fully appreciate the frustration and depression the condition engendered in its victims and the benefits that could arise from reversing it.
Along the way, he met resistance from religious conservatives who insisted that life must begin only through intercourse, not artificially, and from fellow scientists who resented the fact that he spoke frequently with the media about both his research and the ethical implications.
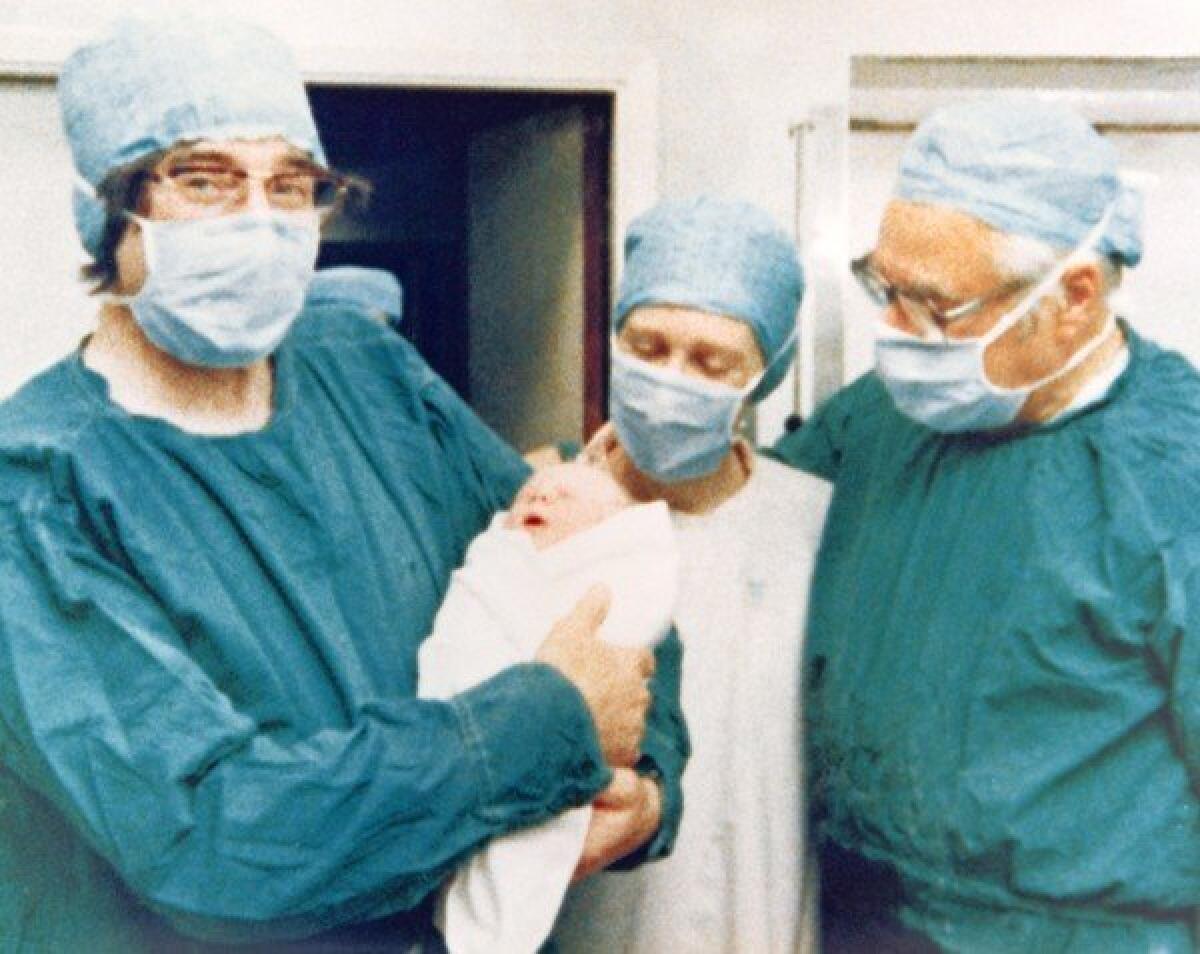
On July 25, 1978, after two decades of intensive research, Edwards and his colleague, Dr. Patrick Steptoe, announced the birth of Louise Joy Brown, the first infant born from an egg fertilized outside the human body. That seminal event, the world’s first “test-tube baby,” triggered the age of in vitro fertilization (IVF), a process that has led to more than 5 million births worldwide and dramatically altered the reproductive landscape.
Today, about 350,000 IVF babies are born each year to infertile couples, single people and gay and lesbian couples. The technique also allows for preimplantation genetic diagnosis, in which potential birth defects are identified before the fertilized egg is implanted.
The feat won Edwards the 2010 Nobel Prize in Physiology or Medicine – Steptoe died in 1988 and was thus ineligible – and a 2011 knighthood “for services to human reproductive biology.”
Edwards died in his sleep Wednesday at his home near Cambridge, England, following a long illness, according to officials at the University of Cambridge, where he worked in the department of physiology. He was 87.
To the layman, IVF might seem no more complicated than adding sperm to an egg in a petri dish and then implanting the resulting embryo in either the mother or a surrogate. But Edwards and his colleagues had to overcome a variety of scientific obstacles before their work bore fruit.
As early as 1935, researchers had shown that a fertilized rabbit egg could pass through the early stages of growth in vitro, and by 1959 it had been shown that such eggs could be implanted in a female rabbit and produce viable embryos. But human eggs proved much more difficult.
The first problem was obtaining eggs. Working with mice, Edwards’ team showed that females could be induced to release many eggs simultaneously by the injection of certain hormones, a process known as super-ovulation. They then showed that the same phenomenon could occur in humans, overturning the previous belief that super-ovulation was impossible in human females.
Mammalian eggs must reach a certain stage of maturity before they can be fertilized by a sperm. Previous researchers had shown that this maturation could occur in vitro for eggs from mice and other small animals, but they failed to observe it with human eggs. Eventually, Edwards deduced that human eggs simply took two or three times as long as mouse eggs to mature in petri dishes.
Another problem lies with the sperm. Many researchers had shown that sperm has to be activated, or “capacitated,” in the uterus before it can penetrate the egg. For a time, Edwards’ team thought they might have to retrieve capacitated sperm from the uterus to achieve IVF, but he and graduate student Barry Bavister eventually demonstrated that the sperm could be activated by increasing the alkalinity of the growth medium in the laboratory.
The potential need to recover sperm from the uterus led Edwards to contact Steptoe, one of the pioneers in the then-emerging field of laparoscopic surgery. Such surgery uses thin tubes and small television cameras and tools to probe inside the human body with minimal incisions, manipulating organs and collecting tissue samples.
That proved to be the crucial technique for safely collecting eggs from women, replacing previous approaches which relied primarily on ovarian tissue taken from infertile women in biopsies.
By 1969, the team had published a paper in the scientific journal Nature showing that human eggs could be fertilized in vitro and that some – two of 56 – could begin to mature. But the nature of his work and Edwards’ extensive interactions with the media offended the scientific establishment, and he was unable to obtain grants. Most of his work for the next decade was supported by private funding.
In 1971, Edwards and lawyer Dave Sharpe published a seminal paper in Nature outlining the ethical issues involved in IVF research and the pros and cons associated with various regulatory responses to it. He clearly foresaw many of the objections to the work that would arise, but chose to continue anyway.
Edwards and Steptoe began implanting fertilized eggs in women in the early 1970s, but more than 100 initial attempts resulted in spontaneous abortions. Eventually, they realized that the hormone treatments given to women to induce super-ovulation and early maturation of eggs were disturbing hormonal balances, producing the stillbirths.
Eventually, the pair decided to collect a single egg that had matured naturally and attempt to fertilize it.
In November 1977, a young couple named Lesley and John Brown came to Edwards and Steptoe after nine fruitless years trying to conceive. Using their newly refined techniques, the team collected, fertilized and implanted an egg in Lesley Brown and on July 25 of the following year, she gave birth to Louise via a Caesarean section. The infant proved to be in perfect health, much to everyone’s relief.
On July 4, 1979, the second test-tube baby, Alistair MacDonald, was born, but skeptical funding agencies continued to refuse funds for research.
Using private donations, Edwards and Steptoe established the Bourn Hall Clinic, the world’s first IVF center, on the outskirts of Cambridge. By 1986, more than 1,000 babies had been born via IVF at Bourn Hall and a similar number in the rest of the world.
Robert Geoffrey Edwards was born Sept. 27, 1925, in the Yorkshire mill town of Batley, where his mother was a machinist. His family moved to Manchester when he was 5 but spent summers in the Yorkshire Dales, where young Bob worked on farms and developed a love for animals.
When he finished high school in 1943, he was drafted into the British Army, where he spent four years, becoming a commissioned officer. In 1948, he enrolled in agricultural sciences at the University College of North Wales at Bangor, but after two years found the course work unscientific and boring. He transferred to zoology and earned his degree in 1951. He then went to Edinburgh University to receive his advanced degree in animal genetics.
He spent a year of postgraduate work at Caltech, then joined the National Institute for Medical Research in London in 1958. He left in 1962 after the institute’s director banned any work in human IVF, spending a year in Glasgow before joining Cambridge University.
Edwards is survived by his wife, the former Ruth Fowler; five daughters; and 11 grandchildren.
More to Read
Start your day right
Sign up for Essential California for the L.A. Times biggest news, features and recommendations in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.






