With an epidemic of mental illness on the streets, counties struggle to spend huge cash reserves

When California voters passed a tax on high-income residents in 2004, backers said it would make good on the state’s “failed promise” to help counties pay for the treatment of the mentally ill.
After nearly 15 years, Proposition 63 — the Mental Health Services Act — has steered billions of dollars to the counties across the state. But huge sums remain unspent at a time when mental illness has become an epidemic among the homeless population.
For the record:
2:40 p.m. Aug. 23, 2018Mental health spending: In the Aug. 19 Section A, an article about the Mental Health Services Act stated that Proposition 2 — the November ballot initiative that would issue $2 billion in bonds for supportive housing for homeless individuals with mental illness — would be repaid using funds from the Mental Health Services Act that counties have not spent. The bonds would be paid using funds before allocation to the counties. Additionally, a previous version of this article said then-state Sen. Darrell Steinberg was the co-author of Proposition 63. Steinberg was an Assembly member at the time.
As of June 2017, $1.6 billion was being held in reserve in nearly three-quarters of the counties in the state. In Los Angeles County, the Department of Mental Health had accumulated nearly $900 million. The unspent funds are believed to have increased in the fiscal year that ended June 30, but figures were not yet available.
Advocates say much of this money could have put crisis teams on the streets, started construction on supportive housing projects and funded psychiatric urgent care centers. According to some estimates, more than a quarter of California’s homeless have a mental illness; in Los Angeles County, the percentage is slightly higher.
“It is shocking to see these large reserves when we have a funding stream to address the crisis that Los Angeles and other jurisdictions are facing,” said Catherine Blakemore, executive director of Disability Rights California.
County agencies are developing plans to draw down these balances.
The L.A. County Department of Mental Health recently proposed spending $896 million in surplus cash on a variety of projects and services, including the construction of a new urgent care clinic at Harbor-UCLA Medical Center and psychiatric mobile response teams.
The budget was adopted by the Board of Supervisors in June, but it is unclear how soon those funds will reach the proposed projects and services. Meanwhile, the reserves continue to earn millions in interest.
“Counties have a lot of funds, and they sometimes struggle to spend the money as fast as it comes in,” said Brian Sala, deputy director of the Oversight and Accountability Commission, which monitors mental health care programs in the state.
‘Poor oversight’
Experts cite a number of factors for these balances: the volatility of the fund, its spending requirements and a lack of guidance from Sacramento.
In a February report, the state auditor faulted the California Department of Health Care Services for “poor oversight” of the agencies statewide that receive these funds every month. Health Care Services, which agreed with most of the auditor’s recommendations, declined to comment for this article.
The money raised by Proposition 63 accounts for 25% of the California’s $8-billion budget for mental health programs, and in the last six years, the administration of this money has been routinely criticized.
In 2012, the state auditor targeted the law’s former administrator, the Department of Mental Health, for its lack of oversight. Two years later, the Little Hoover Commission cited poor record-keeping for the lack of evidence that the law had helped Californians with mental illness.
Advocates say the administrative bottlenecks at the state and county level are thwarting treatment for distressed, psychotic or depressed Californians who are at risk for suicide, incarceration or chronic hospitalization.
“Why are we taxing millionaires if we’re not good stewards of this fund?” said Brittney Weissman, executive director of the L.A. chapter of the National Alliance on Mental Illness.
Revenues rose, budgets stayed flat
Rusty Selix, who co-authored Proposition 63 with then-Assemblyman Darrell Steinberg, said he knew “something was wrong” almost four years ago when he served as a policy consultant with the California Council of Community Mental Health Agencies.
The state was coming out of the recession and revenues were climbing, but agencies contracted by the counties to provide service were not seeing their budgets increased.
“When revenues are going up, there is a tendency to underestimate how much growth is really happening,” Selix said. “Counties didn’t accurately account for all the money that was coming in.”
Some counties held onto funds that should have been returned to the state after three years, if Health Care Services had been enforcing that requirement of the law.
Local administrators saw the rising balances as a way to protect programs already in place from the law’s funding volatility.
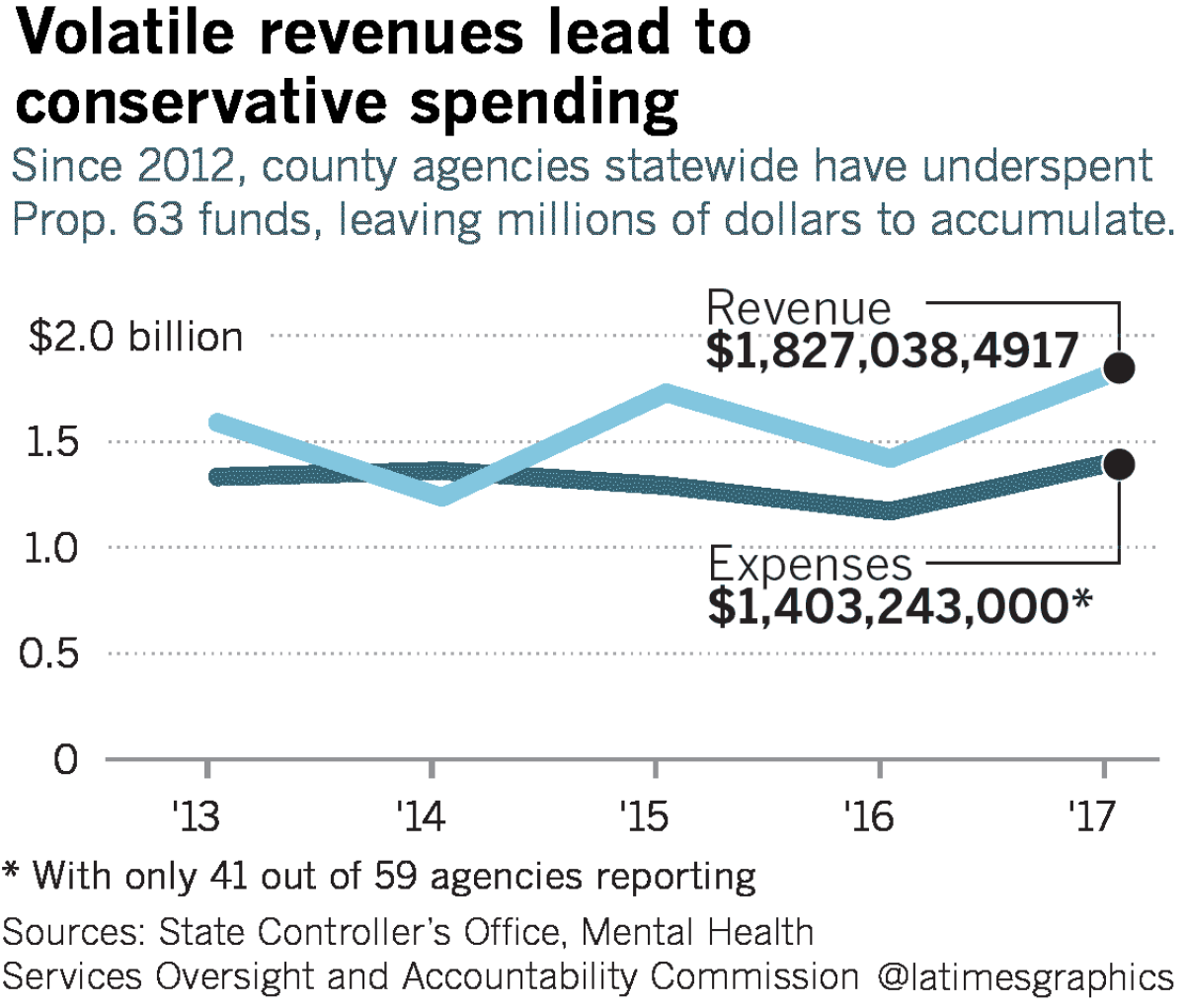
Rising and falling on the fortunes of people earning at least $1 million a year, Proposition 63 revenues rely upon the strength of California’s economy. From 2013 to 2016, revenues dropped 22%, rose 40% and fell 18%.
During prosperous years, counties received more money than they had budgeted for, and because this windfall couldn’t be guaranteed in following years, administrators were reluctant to spend it on projects that require sustaining funds.
The law, however, has safeguards when revenues drop. Counties are given three years to spend the money, while other appropriations must be spent or committed within a year or two.
“You don’t want to force the system to work at breakneck speeds to spend in unwise ways,” said Sala, of the state oversight panel..
Counties are also required to maintain a rainy-day fund — a “prudent reserve” — to pay for programs during years when revenues fall.
State guidelines do not specify an amount but initially recommended that counties set aside at least 50% of their largest annual expense. L.A. County’s rainy-day fund has averaged $160 million over the last five years.
In addition to the prudent reserve, counties have also built up separate cash stockpiles. By the end of the 2016-17 fiscal year, state mental health departments held a combined prudent reserve of $286 million and a separate cash balance of $1.48 billion.
L.A. County’s cash reserve at that time was $893 million.
“There clearly is an issue with cash management policies in many counties,” Sala said.
Complexity, caution fuel cash buildup
The unspent funds have accumulated, in part, because of the complexity of the Mental Health Services Act itself, experts say. Each of the law’s five components follows a different set of rules, planning requirements and approval mechanisms, and money can be spent only after an extensive approval process.
Counties submit plans to stakeholders in the community — families, individuals with mental illness — then to the Board of Supervisors, and in the case of innovation, to the Oversight and Accountability Commission.
Marvin Southard, who headed L.A. County’s Department of Mental Health until his retirement in 2015, said the process hobbled his effort to open more psychiatric urgent care centers. “If the money had been more secure or the rules for utilizing it easier to navigate, we would have opened those faster,” he said.
But political caution also plays a role.
Local officials have tried to cushion essential programs from sharp revenue swings, which in down years can lead to layoffs and reduced services — and be a political liability for elected boards of supervisors.
These local programs, provided by agencies contracted by the Department of Mental Health, “are the core of the [law]. These are the clients that we have for years,” Southard said.
Funding for these ongoing programs has not grown proportionally with the counties’ revenue gains, and cash reserves have soared.
Yoga, hikes and an amusement park ride
Proposition 63 also requires counties to develop programs aimed at preventing the progression of severe mental illness. Allocations in the past — yoga, horseback riding, wilderness hikes — have been criticized, prompting counties to take a more conservative approach.
The law also encourages innovation: “novel, creative and/or ingenious mental health practices/approaches that contribute to learning.” In 2013, Orange County officials proposed spending $2.2 million on an amusement park ride into the brain, to highlight the origins and treatment of some mental disorders. It was initially approved by the Board of Supervisors but hasn’t been developed.
While only 5% of money coming in under Proposition 63 goes toward innovation, counties have consistently spent far less. From 2012 to 2017, Los Angeles County received $114 million for innovation and spent $68 million.
“We’re asking public officials to take risks with public dollars,” said Toby Ewing, executive director of the Oversight and Accountability Commission. “When that doesn’t work out, public officials are punished.”
To address the surplus funds and lack of guidance from the Department of Health Care Services, politicians have come up with a series of legislative fixes.
Assembly Bill 114 — passed in 2017 — allowed counties to keep $230 million in cash reserves if they came up with a spending plan by June 30 that would be executed by June 2020. Los Angeles County claimed nearly $90 million of that amount in its 2018-19 spending plan.
This year, Senate Bill 1004 — currently being considered in the Assembly — would require the Oversight and Accountability Commission to play more of a role in reviewing and approving prevention and early intervention programs.
Finally, in November, voters will decide on Proposition 2, which would allow the state to issue $2 billion in bonds for permanent supportive housing for chronically homeless people with mental illness. The bonds would be repaid over the years using approximately 7% of the counties’ unspent reserves.
Each measure represents a piecemeal approach to the structural problems of the law.
Some officials cite a lack of leadership in Sacramento and criticize the decentralization of mental health care services in California that has isolated local governments, mental health boards, clients and their families.
The law, said Jonathan Sherin, head of L.A. County’s Mental Health Department, is “not set up in a way that is complementary, that creates synergy and gets the money from the taxpayers, the millionaires, out into the streets.”
Twitter: @tcurwen
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.











