As health officials turn increasingly toward wastewater testing as a means of tracking the spread of H5N1 bird flu among U.S. dairy herds, some researchers are raising questions about the effectiveness of the sewage assays.
Although the U.S. Centers for Disease Control and Prevention says current testing is standardized and will detect bird flu, some researchers voiced skepticism.
“Right now we are using these sort of broad tests” to test for influenza A viruses in wastewater, said epidemiologist Denis Nash, referring to a category of viruses that includes normal human flu and the bird flu that is circulating in dairy cattle, wild birds, and domestic poultry.
“It’s possible there are some locations around the country where the primers being used in these tests ... might not work for H5N1,” said Nash, distinguished professor of epidemiology and executive director of City University of New York’s Institute for Implementation Science in Population Health.
Answering the basics on Bird Flu 2024
The reason for this is that the tests most commonly used — polymerase chain reaction, or PCR, tests — are designed to detect genetic material from a specific organism, such as a flu virus.
But in order for them to identify the virus, they must be “primed” to know what they are looking for. Depending on what part of the virus researchers are looking for, they may not identify the bird flu subtype.
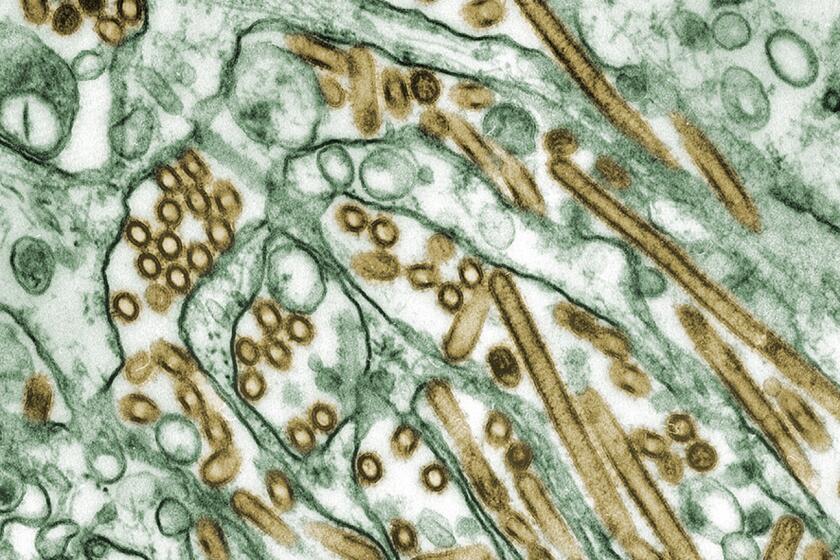
There are two common human influenza A viruses: H1N1 and H3N2. The “H” stands for hemagglutinin, which is an identifiable protein in the virus. The “N” stands for neuraminidase.
The bird flu, on the other hand, is also an influenza A virus. But it has the subtype H5N1.
That means that while the human and avian flu virus share the N1 signal, they don’t share an H.
If a test is designed to look for only the H1 and H3 as indicators of influenza A virus, they’re going to miss the bird flu.
Marc Johnson, a professor of molecular microbiology and immunology at the University of Missouri, said he doesn’t think that’s too likely. He said the generic panels that most labs use will capture H1, H3 and H5.
He said while his lab specifically looks for H1 and H3, “I think we may be the only ones doing that.”
It’s been just in the last few years that health officials have started using wastewater as a sentinel for community health.
Alexandria Boehm, professor of civil and environmental engineering at Stanford University and principal investigator and program director for WastewaterSCAN, said wastewater surveillance really got going during the pandemic. It’s become a routine way to look for hundreds if not thousands of viruses and other pathogens in municipal wastewater.
“Three years or four years ago, no one was doing it,” said Boehm, who collaborates with a network of researchers at labs at Stanford, Emory University and Verily, Alphabet Inc.’s life sciences research organization. “It sort of evolved in response to the pandemic and has continued to evolve.”
Since late March, when the bird flu was first reported in Texas dairy cattle, researchers and public health officials have been combing through wastewater samples. Most are using the influenza A tests they had already built into their systems — most of which were designed to detect human flu viruses, not bird flu.
Samples from wastewater plants across the nation show an increase in multiple flu viruses. Some experts worry that H5N1 bird flu might be to blame.
On Tuesday, the CDC released its own dashboard showing wastewater sites where it has detected influenza A in the last two weeks.
Displaying a network of more than 650 sites across the nation, there were only three sites — in Florida, Illinois and Kansas — where levels of influenza A were considered high enough to warrant further agency investigation. There were more than 400 where data were insufficient to allow a determination.
Jonathan Yoder, deputy director of the CDC’s Division of Infectious Disease Readiness and Innovation, said those sites were deemed to have insufficient data because testing hasn’t been in place long enough, or there may not have been enough positive influenza A samples to include.
Asked if some of the tests being used could miss bird flu because of the way they were designed, he said: “We don’t have any evidence of that. It does seem like we’re at at a broad enough level that we don’t have any evidence that we would not pick up H5.”
He also said the tests were standardized across the network.
“I’m pretty sure that it’s the same assay being used at all the sites,” he said. “They’re all based on ... what the CDC has published as a clinical assay for for influenza A, so it’s based on clinical tests.”
But there are discrepancies between the CDC’s findings and others’.
Earlier this week, a team of scientists from Baylor College of Medicine, the University of Texas Health Science Center at Houston, the Texas Epidemic Public Health Institute and the El Paso Water Utility, published a report showing high levels of bird flu from wastewater in nine Texas cities. Their data show that H5N1 is the dominant form of influenza A swirling in these Texas towns’ wastewater.
But unlike other research teams, including the CDC, they used an “agnostic” approach known as hybrid-capture sequencing.
“So it’s not just targeting one virus or one of several viruses,” as one does with PCR testing, said Eric Boerwinkle, dean of the UTHealth Houston School of Public Health and a member of the Texas team. “We’re actually in a very complex mixture, which is wastewater, pulling down viruses and sequencing them.”
“What’s critical here is it’s very specific to H5N1,” he said, noting they’d been doing this kind of testing for approximately two years, and hadn’t ever seen H5N1 before the middle of March.
Blake Hanson, an assistant professor at the University of Texas Health Science Center at Houston School of Public Health and a member of the Texas wastewater team, agreed, saying that PCR-based methods are “exquisite” and “highly accurate.”
“But we have the ability to look at the representation of the entire genome, not just a marker component of it. And so that has allowed us to look at H5N1, differentiate it from some of our seasonal fluids like H1N1 and H3N2,” he said. “It’s what gave us high confidence that it is entirely H5N1, whereas the other papers are using a part of the H5 gene as a marker for H5.”
Boerwinkle and Hanson underscored that while they could identify H5N1 in the wastewater, they cannot tell where it came from.
“Texas is really a confluence of a couple of different flyways for migratory birds, and Texas is also an agricultural state, despite having quite large cities,” Boerwinkle said. “It’s probably correct that if you had to put your dime and gamble what was happening, it’s probably coming from not just one source but from multiple sources. We have no reason to think that one source is more likely any one of those things.”
But they are pretty confident it’s not coming from people.
“Because we are looking at the entirety of the genome, when we look at the single human H5N1 case, the genomic sequence ... has a hallmark amino acid change ... compared to all of the cattle from that same time point,” Hanson said. “We do not see that hallmark amino acid present in any of our sequencing data. And we’ve looked very carefully for that, which gives us some confidence that we’re not seeing human-human transmission.”
The Texas’ team approach was really exciting, said Devabhaktuni Srikrishna, the CEO and founder of PatientKnowHow.com, noting it exhibited “proof of principle” for employing this kind of metagenomic testing protocol for wastewater and air.
He said government agencies, private companies and academics have been searching for a reliable way to test for thousands of microscopic organisms — such as pathogens — quickly, reliably and at low cost.
“They showed it can be done,” he said.