Over 34,000 L.A. County households lost Medi-Cal in July amid rollback of COVID rules

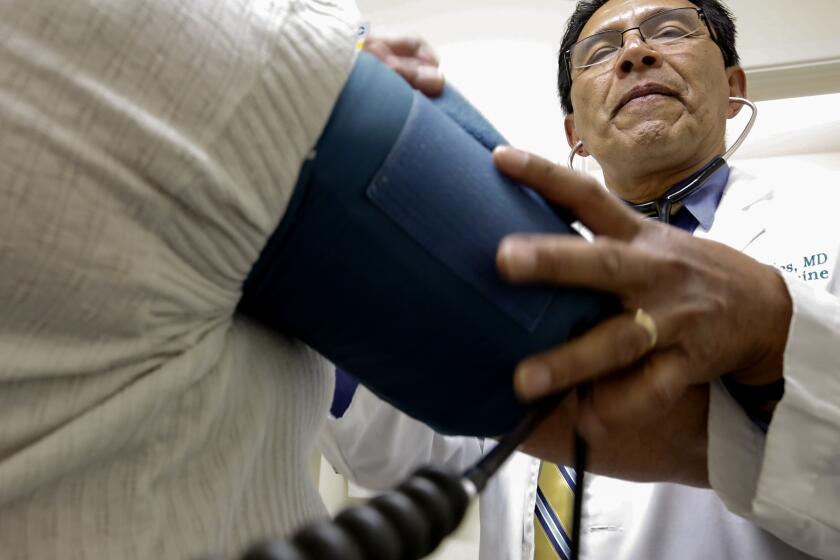
More than 34,000 households in Los Angeles County have had their Medi-Cal coverage discontinued this month as California joins other states in beginning to cut off people from Medicaid programs who no longer meet income requirements or whose paperwork was not submitted in time, according to figures provided by the county.
State officials said Thursday that across California, roughly 225,000 people had been disenrolled this month, the vast majority of whom had not returned the required packets of paperwork. Health officials and legal advocates are closely eyeing such early figures to see how a major shift in health coverage is playing out in L.A. County and across California, amid concerns that people who legally qualify for Medicaid could end up losing it unnecessarily or suffering interruptions in their coverage.
Earlier in the pandemic, federal rules had allowed people to hang on to Medicaid coverage without turning in annual paperwork to prove they were still eligible. Now states have started ejecting people from their programs again after the federal government rolled back those pandemic rules.
Across the United States, more than 3 million people had been booted from Medicaid programs in dozens of states as of Wednesday, according to a KFF analysis. Some people may have lost coverage because they started making too much money to qualify for the government program, but the health policy research group found many had been cut off from Medicaid for “procedural” reasons such as not returning paperwork on time.
Health providers and advocates have warned that people could end up losing coverage even though they are still eligible for Medicaid, due to bureaucratic hiccups such as government mail being sent to an old address. Many families moved during the pandemic, and government agencies may not have current information.
In Los Angeles County, the vast majority of those who lost Medi-Cal — more than 30,000 cases — had their coverage discontinued after renewal paperwork was not marked as received by the county, according to figures presented Wednesday by the county Department of Public Social Services. Each Medi-Cal case handled by the county can include more than one person, so the total number of L.A. County residents affected is likely to be higher.
County officials cautioned that those numbers would continue to shift as they continued to process renewals that were submitted in June. In addition, people who lost their coverage after not returning the required paperwork can still get Medi-Cal reinstated back to when it was cut off, if they turn in the missing materials within 90 days of having their coverage discontinued. After that, they would have to reapply for coverage.
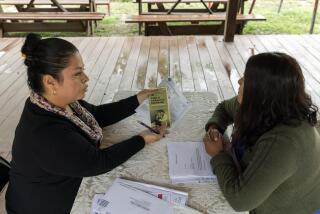
Government officials and community groups are also trying to help people who no longer qualify for Medi-Cal to access other health coverage. Medi-Cal was discontinued in more than 3,800 cases in L.A. County after the county reviewed the information that had been submitted, the county agency said.
Early in the renewal process, “we weren’t seeing a lot of packets coming back. We were getting a little nervous that people just weren’t sending them back,” Jackie Contreras, director of the county Department of Public Social Services, told county officials at a Wednesday meeting.
The good news, she said, is “that has picked up. ... We seem to be building a little bit of momentum.” Contreras said that, so far, the percentage of households losing their Medi-Cal in July appeared to be in the “same range” as was typical before the pandemic.
Across California, state officials said the initial rate of disenrollment has been 21% and is projected to dip to roughly 17% as some Californians get their Medi-Cal coverage reinstated in the coming months. “This would be equal to or better than our disenrollment rate prior to COVID-19,” said Jacey Cooper, chief deputy director of healthcare programs for the California Department of Health Care Services, who added that the state agency was “very happy” with the early figures.
“However, we know that we want to do more to keep people covered and to ensure that they have what they need,” Cooper told reporters.
Legal advocates have raised concerns about whether county agencies handling the process across California are prepared and properly staffed for the deluge of renewal cases they will need to handle over the next year. In L.A. County, Contreras said her department, which has been trying to fill vacancies and grappling with attrition, had made job offers to dozens of people who will fill positions in its Medi-Cal program and start getting trained by the end of July.
Some Angelenos have run into hiccups with a state website where they have uploaded their renewal forms, said Dina Dimirjian, staff attorney at the Health Consumer Center of Neighborhood Legal Services of Los Angeles County. “They might think they’re all set and they could start uploading documents,” but if their online account has not yet been linked to their Medi-Cal case, they could be at risk of losing their coverage despite having tried to turn in their paperwork, Dimirjian said.
“Sometimes people are turning things in, it’s not marked as received, and they see their Medi-Cal terminate anyways,” David Kane, an attorney at the Western Center on Law & Poverty, said during a county meeting.
California will soon require Medi-Cal recipients to prove their eligibility again. But it has a safety net for people who lose their coverage.
Los Angeles County has also had long waits on its phone lines, which means that low-income people who run into problems with their Medi-Cal paperwork could have trouble reaching the county for assistance. At Venice Family Clinic, health insurance program manager Pattie Lopez said the county phone lines were so busy on a recent day that she could not get through to wait on hold, and instead got a message telling her to call back later.
Kimberley Graham, director of patient access at the community health network AltaMed, said its longest wait last week stretched to an hour and 40 minutes. One patient told AltaMed they had tried to phone the county to update their address but gave up because of the long wait, Graham said.
Others have seen the envelope of paperwork from L.A. County and “thought it was a scam,” Graham said. “They just didn’t do anything with it, or they had questions about it.” She was somewhat reassured that many people were bringing the envelopes in to AltaMed clinics to ask about them.
More people are expected to lose coverage over time, as more Medi-Cal cases come up for renewal each month. Nearly 180,000 cases in L.A. County were due back to the county by the end of June. Many families had their coverage automatically renewed as L.A. County checked information against a federal database for other government programs, but roughly 126,000 households had to provide information by the end of last month.
Nearly 180,000 more cases are now due in July. “This is an ongoing process,” Contreras said, telling county officials that her department was open to ideas on “how to most effectively reach out to our communities and our customers and make sure that we keep folks on Medi-Cal in any and every situation where we can.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.