Do I still need to wear a mask indoors? What you need to know about the Delta threat

Los Angeles County residents who are fully vaccinated for COVID-19 have for weeks been largely able to shed their face masks, a potent sign of freedom as the pandemic fades.
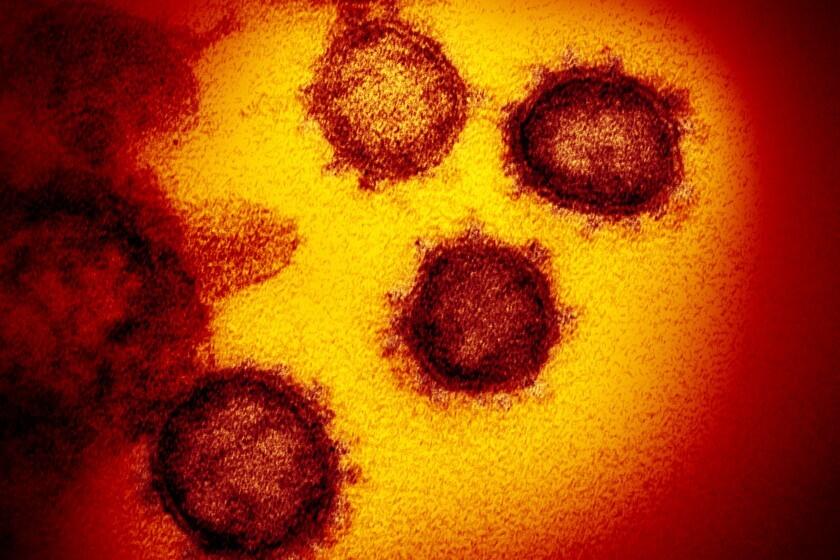
So it came as a shock to some when county health officials on Monday strongly urged even those who have been inoculated to resume masking up indoors as a precaution against the Delta variant of the coronavirus.
So what does this all mean? Here is what you need to know:
Why the change?
Officials are increasingly alarmed by the spread of the Delta variant, which may be twice as transmissible as the conventional coronavirus strains.
While the available COVID-19 vaccines appear to offer strong protection, there’s real concern surrounding the vulnerability of those who have yet to receive all their required shots, or any doses at all.
The Delta variant now makes up 14.5% of coronavirus cases analyzed so far this month in California, up from 4.7% in May.
Delta is now the third most common coronavirus variant in California, new data show.
The variant makes up 14.5% of California coronavirus cases analyzed so far in June, up from 4.7% in May, when it was the fourth-most identified variant statewide, according to data released by the California Department of Public Health.
Experts say the Delta variant, which was first identified in India, poses a greater chance of infection for unvaccinated people if they are exposed. It has been responsible for the rise in cases recently in India, the United Kingdom and elsewhere.
But vaccinated people are well protected against infection and illness. One recent study found that the full two-dose course of the Pfizer-BioNTech vaccine was 88% effective against symptomatic disease caused by the Delta variant and 96% protective against hospitalization.
With the highly contagious Delta variant of the coronavirus continuing to spread statewide, the Los Angeles County Department of Public Health is recommending that all residents wear masks in public indoor spaces — regardless of whether they’ve been vaccinated for COVID-19.
What do we know about Delta in L.A. County?
In L.A. County, 123 people are confirmed to have been infected with the Delta variant thus far. Of those, 110 were unvaccinated and three were partially vaccinated. There were two hospitalizations among people in this group.
Cases involving the variant have been found in 10 fully vaccinated individuals, none of whom ended up needing hospital care.
No one has died from the Delta variant in L.A. County.
Almost everyone who has died in L.A. County of COVID-19 has been unvaccinated.
Data released by the county showed that 99.8% of COVID-19 deaths from Dec. 7 to June 7 occurred among unvaccinated people.
“If you are fully vaccinated, you have a lot of protection,” L.A. County Public Health Director Barbara Ferrer said last week, adding that for the “very small numbers” of people who contracted the Delta variant despite vaccination, “they really did not have serious illness. … This is a pandemic of unvaccinated people.”
In L.A. County, vaccination rates are lower among Black and Latino residents. Health officials fear a disproportionate rise in COVID transmission.
What exactly is the recommendation?
While not a new mask mandate, L.A. County is urging that, as a precaution, “people wear masks indoors in settings such as grocery or retail stores; theaters and family entertainment centers, and workplaces when you don’t know everyone’s vaccination status.”
“Until we better understand how and to who the Delta variant is spreading, everyone should focus on maximum protection with minimum interruption to routine as all businesses operate without other restrictions, like physical distancing and capacity limits,” officials wrote in a statement.
How bad can Delta get?
Many experts don’t expect another COVID-19 surge on the magnitude of those that hammered the state last summer and over the fall and winter — largely because the current level of vaccine coverage is so high.
More than 3 in 5 Californians have gotten at least one vaccine dose to date, but only about half are fully vaccinated, according to data from the U.S. Centers for Disease Control and Prevention.
However, communities with lower vaccination levels do remain exposed to potential outbreaks. That’s especially the case in a now-reopened California, where many of the safety protocols that long defined the state’s coronavirus response — like widespread mask wearing, physical distancing and capacity limitations in businesses and venues — have been lifted.
“I have no doubt that we’ll see some places that are [largely] unvaccinated that are going to have an outbreak,” Dr. Mark Ghaly, California Health and Human Services secretary, said in a talk with the Public Policy Institute of California. “And that’s going to have real consequences.”
Although health experts see reason for confidence as California ends many COVID restrictions, here are some dangerous health scenarios they’ll be watching out for.
Another concern is that every new infection gives the coronavirus additional chance to mutate, potentially in dangerous ways that could increase its infectious potential or reduce vaccine efficacy.
Data released by California show that the percentage of the tested population who have antibodies to the coronavirus — a sign of immunity to COVID-19 — is also increasing.
From May 16 to June 12, 85.9% of Californians who were tested for coronavirus antibodies had them — a promising sign of growing immunity, either because of immunization or past exposure to the virus. That’s up from 76.6%, calculated during a four-week period in May.
Experts have estimated that 70% to 85% of a population needs to have immunity for a region to develop “herd immunity” to COVID-19, which interrupts the sustained transmission of the virus.
It’s unclear whether Delta-plus is more transmissible than the original, highly transmissible Delta variant. Without more research, it shouldn’t yet be cause for alarm, experts say.
Officials are continuing to urge everyone to be vaccinated against COVID-19, including people who survived a previous infection. Experts say immunity provided by the vaccination is more robust and longer-lasting than immunity from an infection.
The highly infectious Delta variant is making the task of getting to herd immunity more difficult.
With conventional coronavirus strains, it could take perhaps 71% of the population to be immune for a region to reach herd immunity and interrupt the virus’ transmission, said Dr. George Rutherford, a UC San Francisco epidemiologist. But a variant such as Delta — because it is so transmissible — would increase that threshold to, say, 84%, he said.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.