California coronavirus deaths double, with rural areas and suburbs hit hard
California’s second surge of the coronavirus has resulted in a near doubling of weekly deaths since the spring — with almost 1,000 fatalities in the last week alone — and radically shifted the geography of the outbreak, a Times data analysis found.
Suburban and agricultural areas that had been relatively spared during California’s first surge of the virus are now being ravaged. And urban areas such as Los Angeles County and the San Francisco Bay Area are reporting fatality numbers just as high, if not higher, than in the spring.
The Central Valley has become home to one of the worst coronavirus hot spots in the country.
In eight southern Central Valley counties, weekly COVID-19 deaths have jumped from about 20 a week in April to nearly 200 a week in the last two weeks, a Times analysis found. San Joaquin Valley residents make up 20% of recent deaths statewide, even though they account for about 10% of the state’s population.
For the seven-day period that ended Monday, 969 deaths were reported across California, the largest weekly death toll since the pandemic began. During the springtime surge of the virus, the highest weekly death toll was during the week of April 21, when 553 deaths were reported.
In the southern part of the state, suburban regions are also experiencing a surge in deaths. San Bernardino County recorded 128 coronavirus fatalities in the seven-day period that ended Monday, almost quadruple the weekly death toll of 34 the week before. Riverside County’s weekly death toll of 83 last week was about double what it was in April.
Orange County tallied 73 deaths last week; for the week of April 21, Orange County recorded six deaths. Ventura County recorded 16 deaths last week; that county reported fewer than five deaths a week in April.
But, overall, perhaps the greatest cause for concern is the Central Valley.
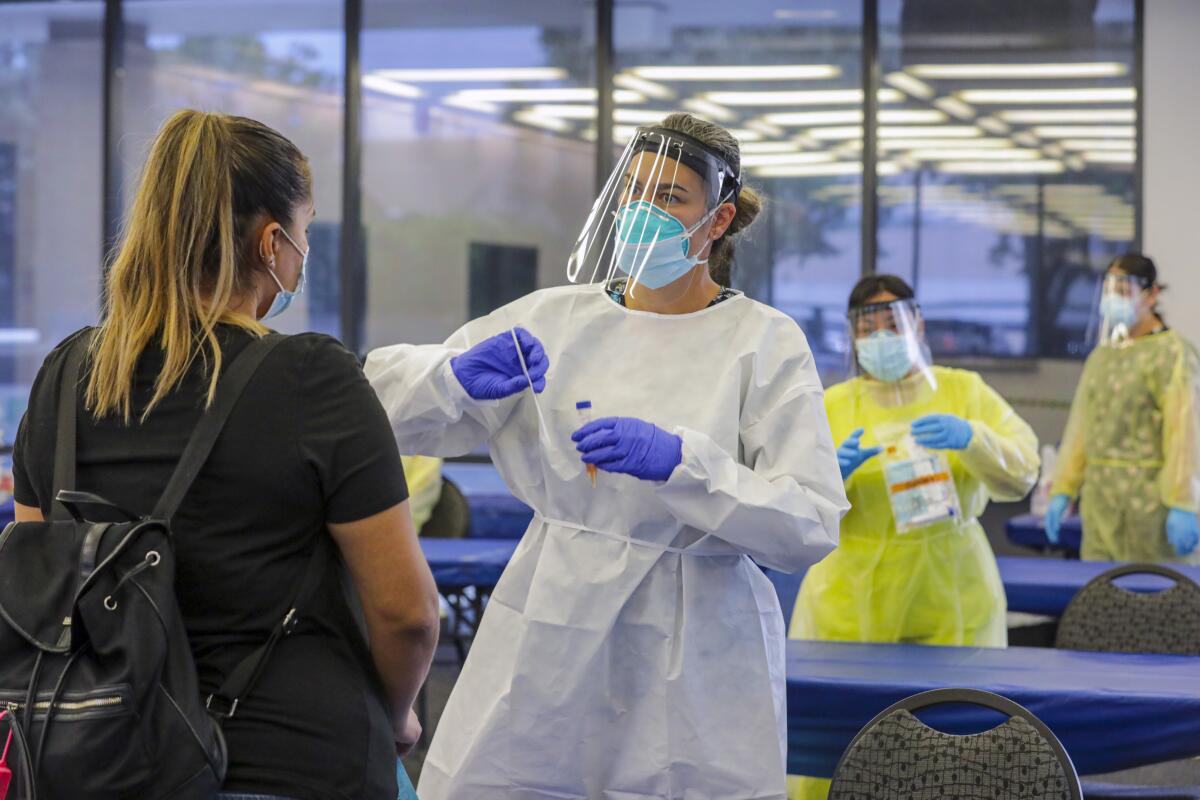
The worsening death toll comes as the coronavirus has spread rapidly among low-wage essential workers in jobs such as agriculture and food processing. Major outbreaks have been reported at a Foster Farms poultry processing plant in Merced County; Central Valley Meat Co., a meatpacking facility in Kings County; and Ruiz Foods, a frozen-food packager in Tulare County.
It’s clear why the San Joaquin Valley is being adversely affected, said Edward Flores, a sociology professor with UC Merced’s Community and Labor Center: The region has an extraordinary number of residents who work as low-income, frontline workers, people with precarious job security in a region notorious for violating workplace safety rules.
“All of these issues ... existed before the COVID pandemic. And just like any other inequality, it’s just gotten bigger now,” Flores said. “It was there before — people were dying on the job; people were losing limbs. ... Now that there’s a pandemic, those agencies are probably going to be even more overwhelmed.”
An analysis by the labor center found that 34% of employees in the San Joaquin Valley work in frontline jobs where there is an increased risk of contracting COVID-19 because employees can’t work from home. More than 40% of workers in Madera County are essential workers — making it the county with the third-highest share of these workers of any other county nationwide.
By contrast, about 18% to 22% of employees in L.A., Orange and San Diego counties and the Bay Area work in frontline essential jobs, such as in agriculture, mining, food manufacturing, grocery retail, transportation, warehousing and healthcare.
Part of the problem, Flores said, is that many of the existing COVID-19 health policies “do little for low-wage workers that ... can’t afford to take time off from work without risking starving or being evicted.”
Although efforts have been made statewide to give more days of paid leave to workers in the food industry, Flores says he wonders how much workers — especially those in the country illegally — know about those rights and what happens if they are fired when trying to follow the rules.
“Employers have a role in this, and they’re just absconding their responsibilities in the name of trying to make a quick profit,” Flores said, citing employers who have threatened workers that they’ll lose their jobs if they miss work. “As long as we want food on our table, there’s going to be people working in some amount of proximity to each other — not just Skyping or Zooming from home — and our policies need to address that.”
Flores said two major things needed to be done: guaranteeing workers get paid if they became infected or needed time off to take care of a loved one, and improving and enforcing health and safety standards at workplaces.
José Roberto Álvarez worked at one of several food distribution facilities briefly closed by officials after the county said they failed to report COVID-19 outbreaks.
The recent outbreaks also have been fueled by some of the most disastrous prisoner transfers in California history.
State officials unwittingly transferred infected prisoners from the California Institution for Men in Chino and seeded new cases at Corcoran State Prison in Kings County and triggered an especially devastating outbreak at San Quentin State Prison in Marin County. The San Quentin outbreak has resulted in the deaths of 25 prisoners and one guard to date, and has filled hospital beds throughout the Bay Area.
After the initial transfer, infected inmates from San Quentin were then shipped to a prison in Lassen County, fueling outbreaks in California’s rural northeast.
An outbreak at Avenal State Prison has been blamed for infecting staff who live throughout the Central Valley, worsening disease transmission in Fresno and Kings counties.
To contain the spread of COVID-19, parks, restaurants and stores are slowly reopening.
Health experts said that some states moved too quickly to reopen society after the first wave of coronavirus cases. Gov. Gavin Newsom, under pressure to lift months-long stay-at-home restrictions in May that had closed vast swaths of the economy, began allowing counties to reopen businesses before meeting his own previously established criteria to reopen safely.
Without naming specific states, Dr. Anthony Fauci, the U.S. government’s top infectious diseases expert, said at a Brown University School of Public Health forum last week that some leaders “skipped over some of the checkpoints” recommended for a safer reopening and loosened stay-at-home orders without waiting for new cases to go down. Outbreaks began spreading at workplaces, and viruses were transmitted at barbecues, parties and bars.
The regions of California hit hardest in the earliest phase of the pandemic — the Bay Area and L.A. County — have seen weekly deaths return to — or exceed — springtime levels.
L.A. County‘s weekly death tally in the spring peaked at 329 in late April, then dropped as low as 194 in late June before climbing as high as 327 two weeks ago and 296 last week.
The Bay Area has seen a death tally worse even than its springtime levels. The region recorded as many as 67 deaths in a single week in April; two weeks ago, the Bay Area recorded 81 deaths. Last week there were 72 fatalities.
San Diego County recorded its two worst weekly fatality counts in mid-July, tallying an average of 56 weekly deaths over two weeks — more than double its April average. In the last two weeks, weekly fatalities are averaging about 31 a week.
Other counties with a sharp growth in recent COVID-19 deaths include Sacramento, Santa Barbara and Sonoma. California’s cumulative COVID-19 death toll is more than 10,600.
Coronavirus cases among children and teenagers are surging in California, up 150% last month, a rate that outpaces COVID-19 cases overall and establishes minors as a small but growing share of the state’s COVID-19 cases.
Still, officials are expressing a note of optimism: Weekly cases and hospitalizations appear to have hit their second peak, even when factoring in a glitch in the state’s reporting system for new cases that was being resolved over the weekend.
Last week, there were an average of 5,816 people in hospitals every day with confirmed coronavirus infections statewide, the second consecutive week there was a decline. The number hit its highest point three weeks ago, when an average of 6,941 people were in the hospital daily in a seven-day period.
Although the statewide average is decreasing, not all regions have seen a decline in hospitalizations. The seven-county Sacramento area has recorded 11 straight weeks of increasing hospitalizations.
Amid the latest surge, elected officials have said they intend to learn from the past in considering future reopening plans.
“We all can see, in retrospect, that some things did open up too quickly, that we didn’t stick with the methodology of do-something-and-wait-three-weeks and see the effect,” Los Angeles Mayor Eric Garcetti said on July 22. “It became kind of a domino effect with the ... irrational exuberance of everybody thinking we could rush back to normal.”
Times staff writers Hailey Branson-Potts, Kim Christensen, Taryn Luna, Luke Money, James Rainey, Jake Sheridan and Richard Winton contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.