Large workplaces are vulnerable to coronavirus super-spread as economy reopens, experts warn

Even as the economy begins to reopen, the coronavirus will remain a threat for some time to come, experts say.
And of particular concern are large workplaces.
Experts say so-called super-spreading events could become a leading cause of virus transmission. Having people clustered together at work could set the stage for large numbers of people falling ill, as happened when 52 workers became infected at a Safeway distribution center in the San Joaquin Valley.
At a panel discussion Wednesday, the former head of the U.S. Food and Drug Administration talked about getting back to work “differently” in the face of an infection that could be with us for the long haul.
Dr. Scott Gottlieb, commissioner of the FDA from 2017 to 2019, said, “People rightly want to know when this is going to be over. And the answer is: It might not be over for a very long time until we’re able to more fully vanquish this pathogen with our technology.”
The virus, he said, could be “with us in perpetuity” but become “something that we can live with, and that we can conquer with vaccines and with therapeutics. But in the interim ... we’re going to need to define a new normal.”
The Los Angeles Times will provide around-the-clock updates on COVID-19 from across Southern California and around the world.Tracking the coronavirus in California: latest numbers | Support our journalism with a subscriptionHave a question about coronavirus? Send us your questions here. | You also can sign up for our newsletterSee latest photo galleryCoronavirus updates for May 13 are here
This new normal, he said in the webinar hosted by the American Public Health Assn. and the National Academy of Medicine, involves allowing society to get back to work and back to the things we enjoy, “but we’re going to have to do so differently.”
“We’re going to have to sacrifice certain trappings and impose certain things that will make life different,” Gottlieb said, “and we’re gonna have to do things more safely than we’ve done before, and with more awareness to the risk of viral transmission.”
There are some positive signs of progress, he added. Gottlieb said New York was experiencing sharp declines in disease, and there is improvement in hard-hit cities including New Orleans, Detroit and Boston.
But there will need to be a marshaling of resources to fight this virus, he said.
As of Thursday, more than 297,000 have died worldwide after being infected with the coronavirus, according to Johns Hopkins University. In the U.S., more than 84,000 fatalities have been reported, including over 2,900 in California, which has reached a stubborn plateau in COVID-19 deaths. The Golden State has been reporting an average of 500 deaths weekly over the past month.
Some experts worry the worst may be yet to come, with perhaps 147,000 deaths nationally and more than 5,800 in California by early August, according to one influential forecast published by the University of Washington’s Institute for Health Metrics and Evaluation.
Dr. Anthony Fauci, the nation’s top infectious disease expert, warned Congress on Tuesday that states that pushed too quickly to reopen businesses could “trigger an outbreak that you may not be able to control.”
Ousted director testifies that Trump has no plan and unrealistic timetable for a coronavirus vaccine
Rick Bright testifies before the House Committee on Energy and Commerce’s health subcommittee after he filed a whistle-blower complaint.
And in testimony prepared for Congress, Rick Bright, an immunologist who says he was ousted from his job overseeing drug and vaccine development at the U.S. Department of Health and Human Services, warned that the world was facing “a great public health emergency, which has the potential to eclipse the devastation wrought by the 1918 influenza which globally claimed over 50 million lives.”
“While it is terrifying to acknowledge the extent of the challenge that we currently confront, the undeniable fact is there will be a resurgence of the COVID-19 this fall,” Bright said. Without a national, coordinated response to the pandemic, Bright said, “2020 will be the darkest winter in modern history.”
A vaccine is likely 12 to 18 months away. It’s possible there could be a very large coronavirus outbreak in the fall, potentially spreading further as students return to school, experts say.
Gottlieb said there must be a focus on at-risk communities, helping people who lack access to testing and good care because of where they work and live, which puts them at higher risk of infection.
And there needs to be investment in staffing up teams of disease investigators to tamp outbreaks, he said.
Blacks, Latinos, Native Americans and Pacific Islanders are among the communities hit hard by the pandemic.
Here are three things experts on Gottlieb’s panel voiced concerns about as the pandemic continues:
Super-spreading events may be responsible for most infections
New Zealand, which has done an excellent job of keeping the coronavirus from becoming a major disaster, discovered that half of all disease transmission came from large transmission events in that country, said Dr. Chris Murray, director of the University of Washington’s Institute for Health Metrics and Evaluation, the publisher of an influential pandemic forecast.
“And that really, I think, puts the onus on employers and local governments keeping the limits on group gatherings down to a pretty small number, like 10 or less, just to avoid the risk of those hundred-people transmission events that we’ve seen quite routinely,” Murray said.
That means that larger workplaces — such as places with assembly lines where people are close to one another — are particularly vulnerable as a threat for rapid spread of disease, said David Michaels, epidemiologist and professor in environmental and occupational health at George Washington University and assistant secretary of Labor for the Occupational Safety and Health Administration in the Obama administration.
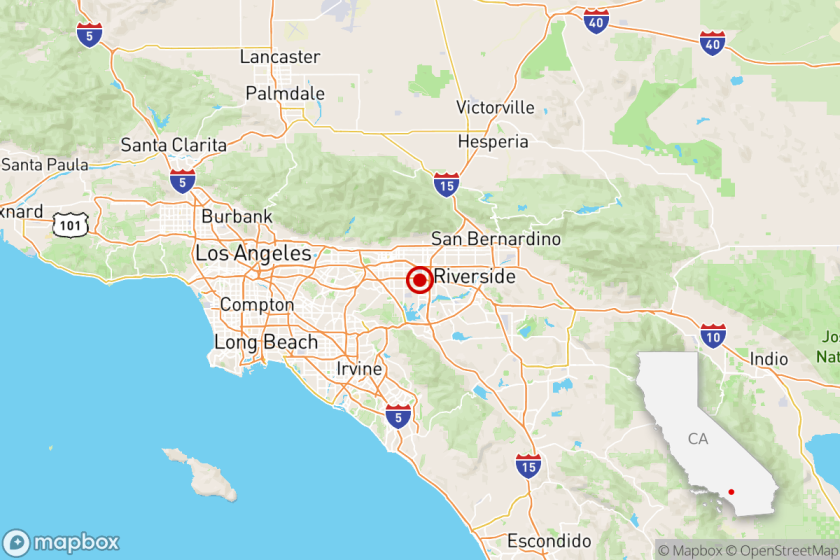
California and the West Coast have already seen a number of mass disease transmission incidents that spread the coronavirus, which scientists call SARS-CoV-2.
The deadly outbreak among members of a choir has stunned health officials, who have concluded that the virus was almost certainly transmitted through the air from one or more people without symptoms.
In Washington state, a single person who was showing signs of illness attended a 2½-hour choir practice at church on March 10 with 60 other people. After the practice, 52 people fell sick with COVID-19, a disease attack rate of 87%, and two died. The virus’ spread was likely facilitated by people being less than six feet from one another and worsened by singing together, according to the U.S. Centers for Disease Control and Prevention.
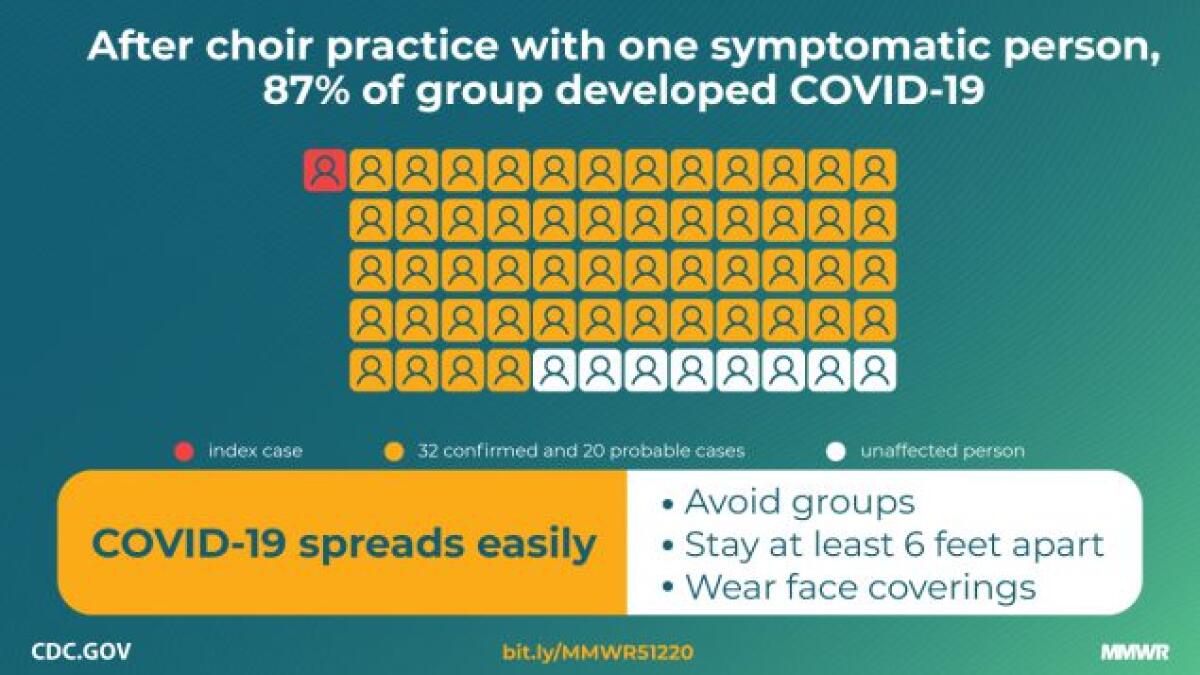
“Certain persons, known as superemitters, who release more aerosol particles during speech than do their peers, might have contributed to this and previously reported COVID-19 superspreading events,” the CDC said in a news release this week. “These data demonstrate the high transmissibility of SARS-CoV-2 and the possibility of superemitters contributing to broad transmission in certain unique activities and circumstances.”
In the San Joaquin Valley, 52 workers at a Safeway distribution center in Tracy, Calif., were found to be infected with the coronavirus, and one worker died. Thousands of people nationwide who work at meat packing plants have been infected, and at least 20 have died. The number of workers at a meat packing plant in California’s Kings County who tested positive for the virus has now risen to 182, the Fresno Bee reported.
To contain the spread of COVID-19, parks, restaurants and stores are slowly reopening.
Workers are at risk
COVID-19 has become a “massive worker safety crisis,” Michaels said. Infection rates are rising rapidly in places where the epidemic is driven by exposure to the virus at work.
But there’s little workplace testing, which he said must become more commonplace.
For instance, he said, there was a coronavirus outbreak in Massachusetts that officials belatedly discovered was associated with a Walmart store and linked to scores of infected employees.
“When the initial cases started to appear, local health authorities had no idea they were all linked to only one workplace. Once they finally put it together, they shut down the store,” Michaels said. “But they said, if they had known earlier … they could’ve gone in there much earlier.”
With no coronavirus vaccine in sight, employers and building landlords are turning to tech, design and distancing to keep office workers healthy.
An outbreak early warning system is needed
As coronavirus testing ramps up, it’s increasingly hard to determine whether an increase in reported cases is simply a result of more widespread testing or if it’s an early sign of a new surge in infections.
That’s a problem, said Murray, of the University of Washington. “What’s the early warning system for the next flare-up or the next hot spot?”
Hospitalizations can serve as an indicator of disease progress. But the problem is, hospital stays are a delayed warning, with an estimated 10-day gap between infection and admission, Murray said.
“So it’s a 10-day lag on what’s happening in the community,” Murray said.
There could be improvements in how hospitals and governments report data. For instance, it would be helpful if every state and county were to report the number of people admitted with COVID-19 to hospitals daily, Murray said, and not just the number of people who are in the hospital.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.