He gave his wife CPR as she died after contracting coronavirus. Officials won’t test him
After more than 30 years in advertising, Loretta and Roddy celebrated their retirement with a trip.
They left their home in Orlando, Fla., for the Philippines on Feb. 4. At one point, they traveled to Thailand. They had layovers in Seoul on the way to the Philippines and the way back to the U.S.
On March 8, they flew into Los Angeles International Airport. They planned to stay at Roddy’s sister’s house in Walnut for two nights and then fly back to Florida on March 10.
What happened next is a nightmarish and ultimately tragic tale of missed signals and bureaucratic stumbling blocks that have shattered the couple’s lives and family.
Loretta, 68, a breast cancer survivor and diabetic, was exhausted after the trip, and the couple wanted to rest and readjust to the U.S. time zone.
The death toll rises to 13 in California and there are more than 470 confirmed cases of the coronavirus.
But on March 9, their children couldn’t get ahold of them until late in the afternoon.
“My dad texted me and my brother and said that he couldn’t wake up mom,” their daughter Rowena said.
“The only thing I remember from the text was him saying my mother didn’t have a pulse,” said Rem, their son, at whose home they lived in Florida.
Roddy tried to revive his wife of 45 years by performing mouth-to-mouth resuscitation and chest compressions. Then he called 911, and an ambulance rushed her to Pomona Valley Hospital Medical Center.
When she arrived, Loretta was unresponsive but had a weak pulse. Hospital workers intubated her and gave her drugs to keep her heart beating. She went into cardiac arrest four times, her family said.
She was placed in isolation, and the Los Angeles County Department of Public Health greenlighted testing for the coronavirus.
Loretta died at 2:57 a.m. March 10. The next day, officials told her family that her test results were positive. Her death was the first to be reported connected to the virus in L.A. County.
But to the family’s shock, the county Department of Public Health did not recommend that 72-year-old Roddy be tested. When he arrived at the hospital March 9, he was isolated and questioned but then discharged.
The latest updates from our reporters in California and around the world
Even after Loretta’s test results came back positive, a doctor from the department told the family that it wasn’t enough for him to have had close contact with a confirmed case of the virus — he must also show symptoms himself, the family said.
“What’s really frustrating is the fact that this is a man who was as close as you can get to the virus and we’re struggling with trying to get him properly tested,” Rem said.
Instead, Roddy has been ordered to self-quarantine for 14 days at his sister’s house, while his family was told to wait and see if he becomes ill.
“I can’t wait,” Rowena said. “I can’t lose both parents in one week.”
The family asked that their last names not be used for fear of being shunned or targeted.
The Los Angeles County Department of Public Health said patient privacy laws prevent it from discussing specific cases. But Bernard Tolliver, a spokesman, said in an email that “all close contacts of confirmed cases are tested if they have any symptoms of respiratory illness.”
The ordeal shows how constraints on testing have caused officials to perform painful and exacting triage, while patients and their loved ones must navigate a maze of bureaucracy to make informed decisions about their care.
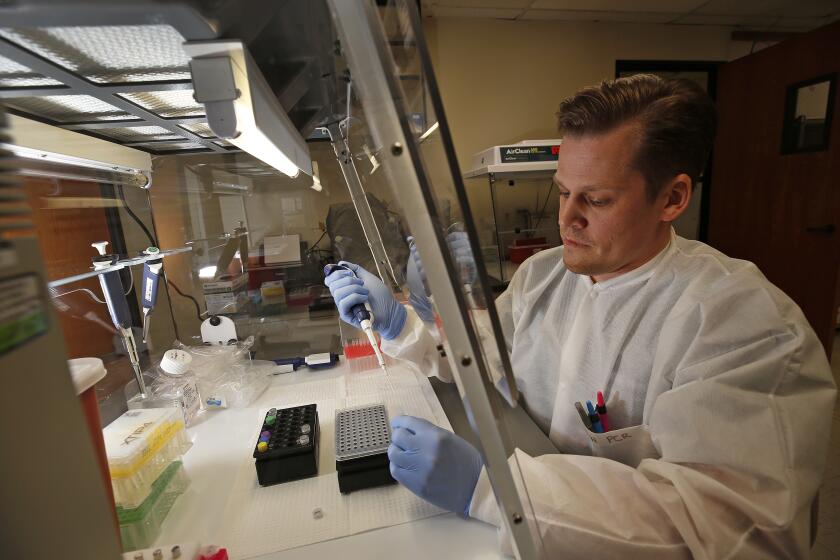
In L.A. County and elsewhere in the U.S., testing has been limited by a shortage of test kits and some chemicals used to process the tests, as well as limited laboratory capacity to process them.
In order for the Department of Public Health to approve sending a specimen to the county Public Health Laboratory for testing, a person must either have a fever or symptoms of respiratory illness and close contact with a confirmed case or work in healthcare; have symptoms requiring hospitalization and a history of travel or certain imaging results; or be part of a cluster of acute respiratory illness within a group living setting like a nursing home or homeless shelter, according to guidelines published by the county Department of Public Health.
Coronavirus tests in California number fewer than 9,000 so far. But officials hope to increase them in the coming days.
If patients don’t fit the county’s criteria for testing, a provider can work directly with a commercial lab to have a test processed there, which gives physicians more leeway to use their clinical judgment in making the decision. But the Department of Public Health still recommends they do so only when a patient has a fever and respiratory symptoms, as well as a risk of exposure.
“I think what it basically comes down to is that the people who really need things aren’t getting them,” said Cathrina, Rem’s wife. “The people who need the tests aren’t getting them. There’s no proper triage in action.”
Roddy, who is a non-insulin-dependent diabetic and takes medication for a cardiovascular condition, is now running a low-grade fever, but his temperature is still not high enough for it to be considered a symptom, his family said.
“Just the other night, I talked to him. ... It’s probably the first time he opened up to me about how he was feeling,” Rem said. “And to hear him say he was confused, he feels so alone and he just wants to come home, it hit really hard.”
“You’re talking about a man that just lost his wife. ... We’ve never experienced anything like this. This is a pandemic that can do this to anybody.”
In another wrinkle, Roddy’s primary care physician is in Orlando. When his family called her and asked her to order testing, she said that she would be required to administer the test herself and could not send one to the L.A. area.
The family also contacted the hospital where Loretta died and asked officials there to have Roddy tested. Hospital staffers said that test kits were scarce there, too, and they could do so only if Roddy were hospitalized in critical condition, the family said.
“The hospital told me and his primary care physician told me, you have to come to terms with the fact that your dad probably has the virus but we cannot do anything about it because there is no cure and we can only give him supportive care,” Rowena said.
However, the family was told that he could receive supportive care only if he tested positive — a frustrating hurdle since he isn’t eligible for testing.
The situation became even more urgent Friday. Roddy’s sister and her husband, who had traveled with Roddy and Loretta for part of their trip, were scheduled to return from the Philippines on a flight to LAX.
Fearing the couple also could be sick, Roddy’s children said they notified the Department of Public Health 24 hours in advance with the couple’s names and birthdates, their airline and when they’d arrive. Public health officials told them the couple would be flagged at the airport and that federal workers would screen them for symptoms of the virus, Roddy’s children said.
No such screening took place. The couple instead got into a taxi and returned to their home, joining Roddy in quarantine, the family said.
All three of them are now self-isolating in Walnut under the supervision of the Department of Public Health, which sends a nurse to take their temperature each day.
For the family, the mountain of red tape has piled onto a heap of troubles.
After officials announced L.A. County’s first coronavirus death at a press conference Wednesday, someone posted to social media Loretta’s full name and the address in Walnut where she had been staying, and where Roddy was in quarantine. The Sheriff’s Department had to assign deputies to monitor the house to ensure it was not targeted, the family said.
The children also had trouble getting much-needed supplies, like Lysol, delivered because websites were sold out and online delivery services were overwhelmed.
Then a crematorium refused to pick up Loretta’s body, saying it hadn’t received clearance from the Department of Public Health. Several phone calls revealed that to be a miscommunication, the family said.
Her body has since been released, but the family is waiting until Roddy is released from quarantine to plan a funeral.
The family emphasized that medical personnel at the hospital have been extremely helpful, as have the nurses and epidemiologists from the Department of Public Health.
“The people who are the boots on the ground are caring and supportive and want to help in every way they can, but they don’t have the resources to help everyone they come in contact with,” Cathrina said. “The big issue is whoever is managing however these tests are distributed ... is not aligned with those who truly need the help.”
By Sunday, Roddy’s brother-in-law was running a fever of 99.8, and the Department of Public Health had recommended that he be tested, the family said. But Roddy’s temperature was 99, still not enough to trigger the recommendation, they said.
Their vacation had been a homecoming of sorts for Roddy and Loretta. The two had met in art school in the Philippines, where they were both born, and moved together to the U.S. to escape martial law imposed on the country in the 1970s. In retirement, they had planned to become “snowbirds,” splitting their time between Cathrina and Rem’s home in Orlando, Rowena’s home in South Carolina, and trips both domestic and overseas.
Now, as their loved ones await the daily updates from Roddy’s nurse, the thought of their father in isolation as he grieves the loss of his wife is almost too much to bear.
“He loved her so much and I can’t even imagine those days where he has to mourn by himself without any of us in quarantine,” Rowena said, her voice catching. “This has all been such a nightmare and to add all these other things on top of it, it’s just absolute insanity. We just want him to come home.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.