Column: Is it too much for patients to expect an itemized hospital bill? Apparently so
Chris Joseph’s 18-year-old son, Jasper, complained that his arms were unusually sore after a workout at the gym a few weeks ago. The pain continued into the next day.
Jasper went with his mother to Providence Saint John’s Health Center in Santa Monica, where a series of tests were conducted. He then returned home.
“Within a half-hour of returning,” Joseph told me, “the hospital called. They said we had to bring our son back now.”
The tests showed Jasper had rhabdomyolysis, which the Centers for Disease Control and Prevention says “occurs when damaged muscle tissue releases its proteins and electrolytes into the blood.”
“These substances can damage the heart and kidneys and cause permanent disability or even death,” it says.
The teen was hospitalized for five nights.
Joseph, 64, told me his son was fine now and that the family had no complaints about his quality of care. But the Santa Monica resident is still scratching his head over the nearly $32,000 hospital bill.
It includes $9,448 in laboratory tests, $6,745 in pharmacy costs, $1,694 for emergency room treatment and $12,368 for five nights in a semi-private hospital room.
“There was very little detail,” Joseph said. “I mean, $6,700 in pharmacy charges? OK, but for what?”
Or, put less delicately, was his son charged $500 for a Tylenol?
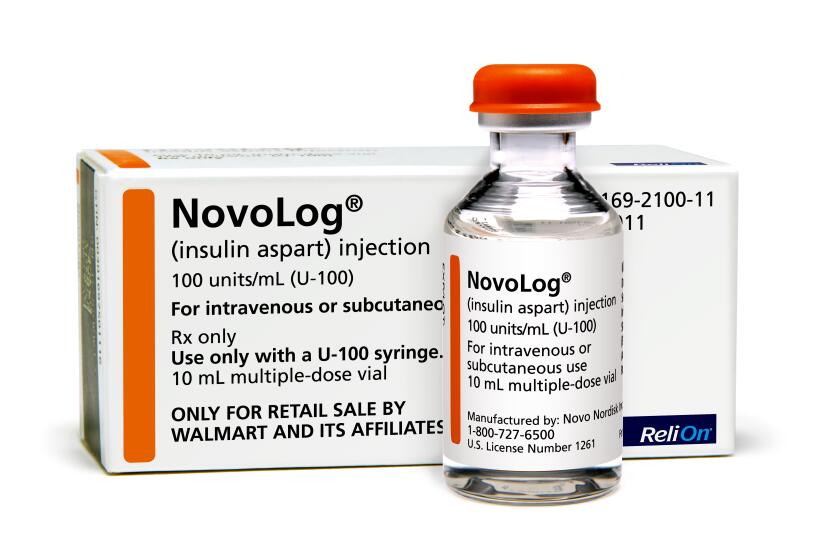
Walmart has unveiled a private-label insulin that sells for about a fifth of what similar insulins cost. Can we expect the same for other drugs?
Joseph called the hospital and conveyed his frustration. A service rep said she’d send an itemized bill within a few days.
“I asked why they don’t just do that automatically,” Joseph said. “She told me that’s just not their policy.”
Patricia Aidem, a Providence spokeswoman, confirmed that itemized bills were only provided when a patient requested one.
Again, Joseph isn’t criticizing the treatment his son received — he’s grateful for all that Providence’s doctors and nurses did for his boy.
“It’s the bill,” Joseph said. “All these charges may be completely legitimate, but consumers should have a right to know what they’re paying for.”
I couldn’t agree more. Lack of billing transparency is one of the core problems with the $4-trillion U.S. healthcare system.
Along these lines, the Biden administration issued a rule last week that aims to minimize surprise bills for emergency care. It’s part of bipartisan legislation passed by Congress last year.
Although, thanks to his insurance, Joseph was responsible for just $2,700 in payments, he’s correct to wonder about the bill’s total cost.
Sky-high medical expenses charged to insurers drive up premiums for all policyholders. The system deliberately masks costs while persistently pushing those costs higher.
“Healthcare pricing is unbelievably opaque — not only to patients but also to providers,” said Mark Duggan, director of the Stanford Institute for Economic Policy Research.
It may cost as little as $100 to manufacture a hearing aid. The list price is typically in the thousands of dollars (and not covered by most insurance).
He told me about the time he sprained his ankle while running and worried that it could be broken. A doctor at an urgent-care clinic “recommended that I purchase a boot, sort of like a ski boot, instead of using crutches.”
Duggan replied that he’d recently switched to a high-deductible insurance plan and would be stuck paying the full cost of the boot.
“Oh, you’ll have to pay for it?” he recalled the doctor saying. “I have no idea what it will cost. But if you have to pay for it, then I would not recommend it.”
The healthcare industry repeatedly tells people that they need to be good medical consumers. That is, they need to make well-informed choices about their treatment.
But if people are denied the information they need to make well-informed choices — or any choice, for that matter — how can they be good medical consumers?
At best, they’re captives to a fog-enshrouded marketplace that goes out of its way to prevent people from knowing how much anything truly costs, or how much money may be changing hands among the various players.
“It’s basic to market functioning that consumers have to know, and agree to, what they are purchasing and what it costs,” said Martin S. Gaynor, a professor of economics and public policy at Carnegie Mellon University.
“Patients can’t be effective consumers if they can’t find out what they’re purchasing and what it costs,” he told me.
A spokesman for the American Hospital Assn. said the industry group “doesn’t have a specific policy on itemized bills.”
But he pointed me toward “voluntary guidelines” issued by the association last year. They say “hospitals should use a billing process that is clear, concise, accurate and patient-friendly.”
That’s not very specific. And, again, it’s just a guideline, not a requirement.
This needs to change. Credit cards can serve as a model.
The Credit Card Accountability Responsibility and Disclosure Act was signed into law in 2009. Among other things, it requires that card issuers provide account holders each month with a clear, concise summary of recent activity.
Card companies have to prominently warn customers about possible late fees and the long-term cost of making only minimum payments each billing cycle. They also must notify cardholders at least 45 days before any changes to interest rates.
The Credit CARD Act was needed because card issuers were notorious for confusing and misleading consumers with monthly statements that hid fees and did nothing to promote responsible behavior, such as paying off balances in a timely fashion.
If lawmakers could step up for cardholders, they can certainly be more attentive to the needs of millions of American hospital patients.
At the very least, medical providers should be required to provide bills that are written in plain English and are accessible to all, and that clearly break out all costs related to treatment.
If that would be too voluminous for a paper bill, doctors and hospitals should provide patients with a secure link to access this information online.
“One thing that makes this very challenging is our incredibly fragmented healthcare system,” Stanford’s Duggan said. “Each hospital and each physician group tends to contract with multiple insurers,” and each insurer might have a different negotiated price for any given treatment.
“The amount of resources and administrative costs that are consumed in negotiating those prices — for many services — is just massive,” he said.
Needless to say, all this lunacy goes away with a Medicare-for-all system that would create a transparent baseline for all medical costs. This is one reason other developed countries are able to deliver healthcare for a fraction of the cost faced by Americans.
U.S. hospitals are already required to list prices for some treatments online, although this is being done in a haphazard, patient-unfriendly way.
If they can’t find the wherewithal to make clear to patients what they’re paying for in bills, they’ll need to be shown the way.
That may be just a Band-Aid for a broken system, but it’s a start.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.