Family and Medical Leave Act and Job-Protected Leave Are Impacted by Mental Health Issues
The National Institute of Health estimates that nearly one in five U.S. adults – or about 52.9 million people in 2020 – live with a mental illness and that only about half receive the help needed.
While many people coping with mental illness may face barriers to treatment that include social stigma, a lack of available services or financial resources, the U.S. Department of Labor is taking measures to ensure that obtaining job-protected leave under the Family and Medical Leave Act is not an additional obstacle to overcome when workers seek mental health support.
The department’s Wage and Hour Division is providing additional resources for workers on their rights to take leave for serious mental health conditions and for employers, HR teams, and legal counsel to better understand how to comply with the FMLA.
An eligible employee may take FMLA leave for their own serious health condition or to care for a spouse, child or parent because of their serious health condition. A serious health condition can include a mental health condition.
Mental and physical health conditions are considered serious health conditions under the FMLA if they require in-patient care or continuing treatment by a healthcare provider, such as an overnight stay in an addiction treatment center or continuing treatment by a clinical psychologist.
The newly published guidance includes Fact Sheet #280: Mental Health Conditions and the FMLA (which can be found at dol.gov) and Frequently Asked Questions on the FMLA’s Mental Health Provisions (also available at dol.gov). The Department of Labor urges employers and their HR and legal teams to learn more about the FMLA and other laws enforced by the Wage and Hour Division, including an online FMLA Compliance Assistance Toolkit, or contact the division’s toll-free helpline at (866) 4US-WAGE (487-9243).
Employees can also call the Wage and Hour Division confidentially with questions, regardless of immigration status, and the department can aid callers in more than 200 languages.
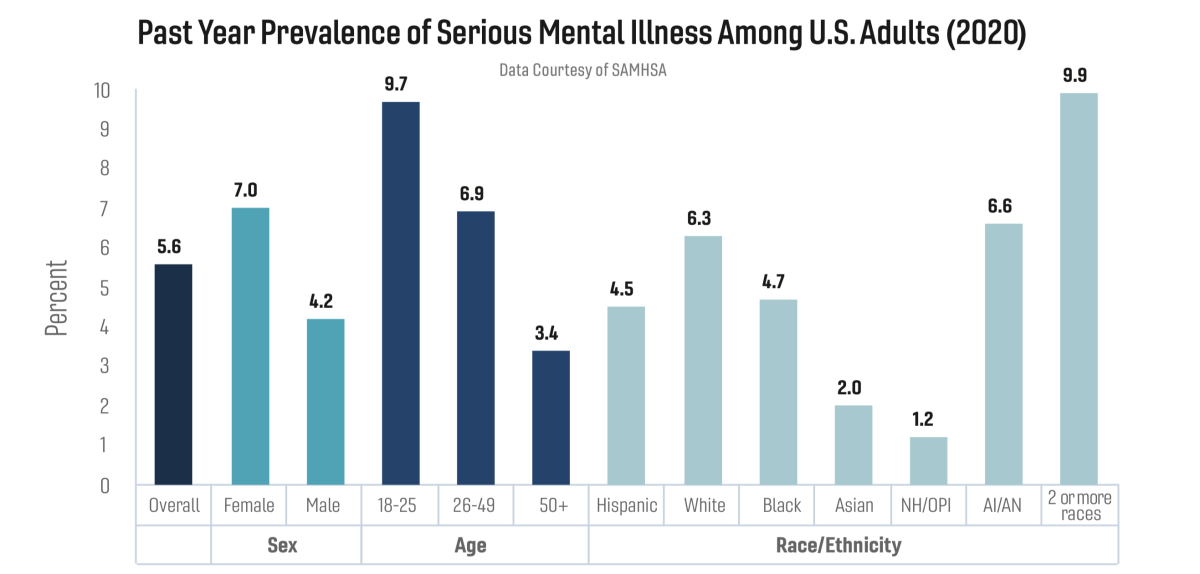
This graphic shows the prevalence of SMI among U.S. adults:
• In 2020, there were an estimated 14.2 million adults aged 18 or older in the United States with SMI. This number represented 5.6% of all U.S. adults.
• The prevalence of SMI was higher among females (7.0%) than males (4.2%).
• Young adults aged 18-25 years had the highest prevalence of SMI (9.7%) compared to adults aged 26-49 years (6.9%) and aged 50 and older (3.4%).
• The prevalence of SMI was highest among the adults reporting two or more races (9.9%), followed by American Indian/Alaskan Native (AI/AN) adults (6.6%). The prevalence of SMI was lowest among Native Hawaiian/Other Pacific Islander (NH/OPI) adults (1.2%).